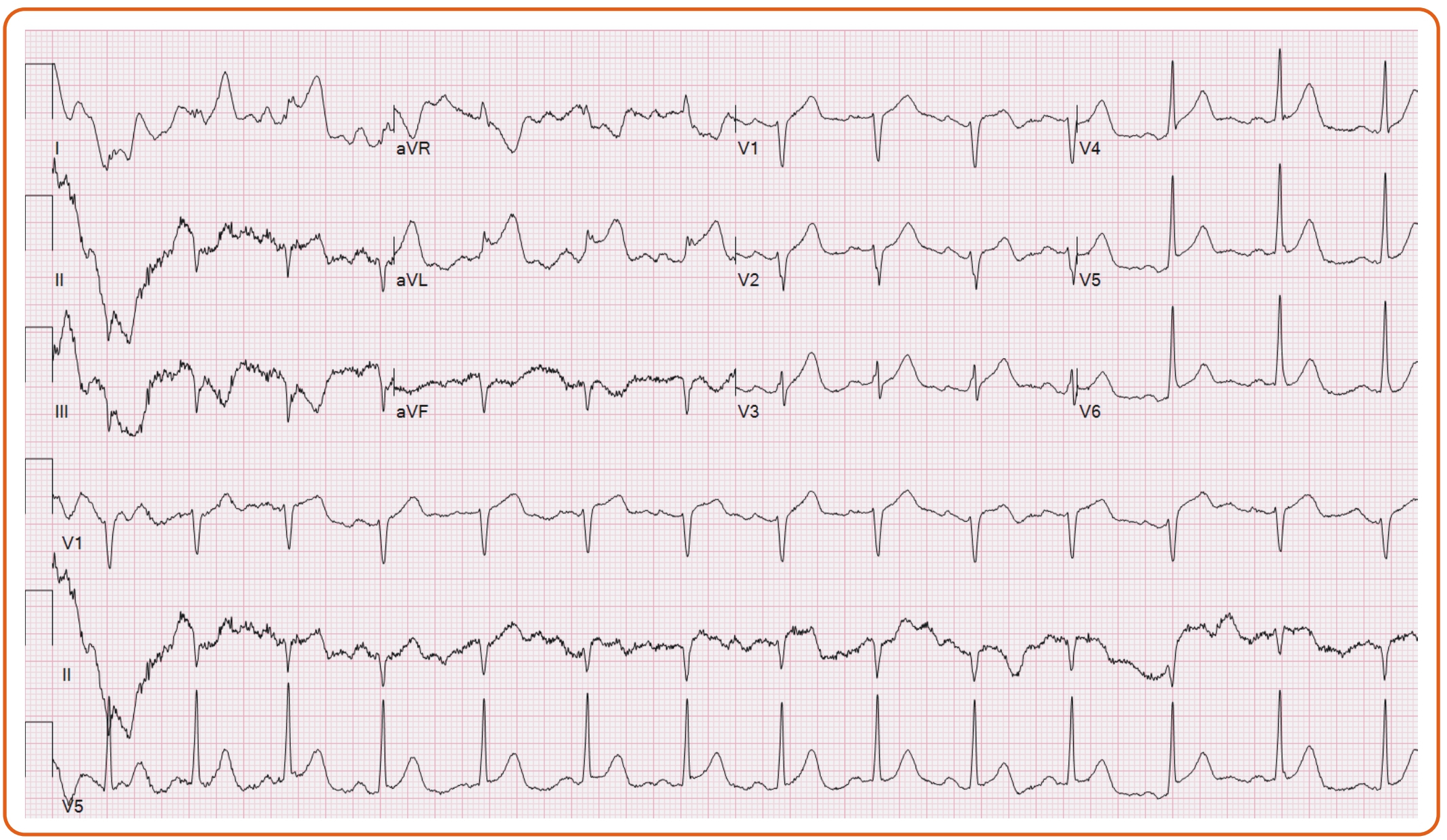
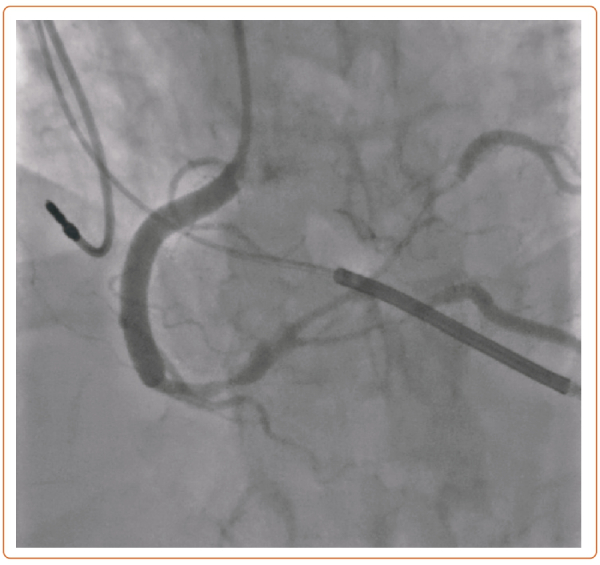
A 55-year-old woman with fibromuscular dysplasia had prior carotid dissection and coronary artery spasm causing cardiac arrest with subsequent implantation of an ICD. After developing a severe migraine, she presented to the emergency department, where she had ventricular fibrillation requiring defibrillation and ST elevations on EKG (Figure 1). She was taken emergently to the catheterization lab, where she was found with severe stenoses involving the right coronary artery (RCA) into the posterior lateral branch (PLB) and posterior descending artery (PDA) (Figure 2).
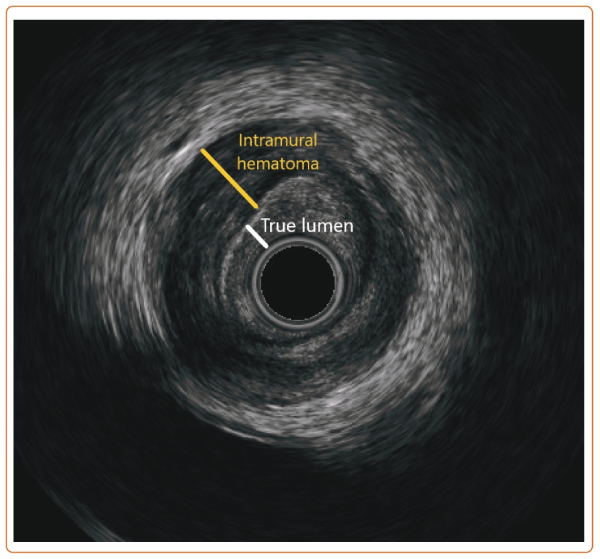
A 6 Fr OptiCross (Boston Scientific) intravascular ultrasound showed a tear in the distal RCA and intramural hematoma involving the PDA and PLB (Figure 3). Although routine revascularization of spontaneous coronary artery dissection should not be performed (class 3), it is reasonable in patients with hemodynamic instability or ongoing ischemia despite conservative therapy (class 2b).1,2
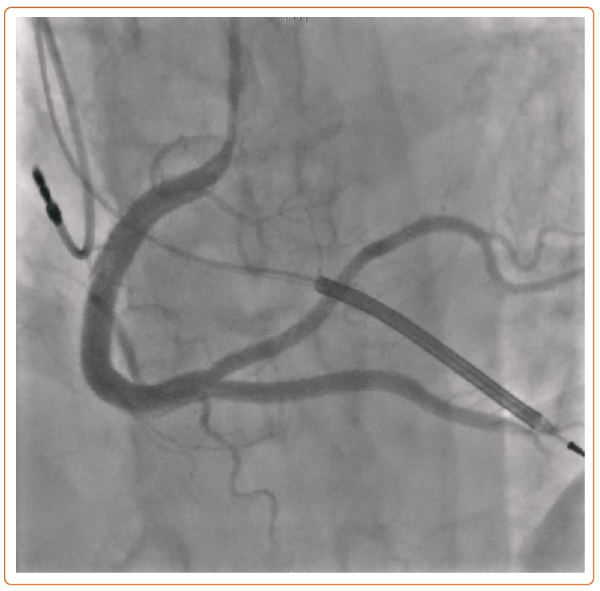
In the setting of her cardiac arrest, progressively worsening flow in the PDA, and ongoing chest pain, we proceeded with percutaneous coronary intervention with drug-eluting stents throughout her RCA, PDA, and PLB.
Because of worsening flow in the PDA, a stent was first deployed in the distal RCA to PDA, then post-dilated proximally. The PLB lost flow, and the intramural hematoma propagated proximally into the mid RCA. Therefore, the mid RCA was stented, and the PLB was rewired, using intravascular ultrasound to confirm true lumen. The PLB was then stented in reverse T and Small Protrusion bifurcation strategy (Figure 4).
She tolerated the procedure without complications and was discharged 5 days post-procedure.