Heart failure with preserved ejection fraction (HFpEF) is a demanding condition for clinicians to manage as it is hard to define, difficult to diagnose and challenging to treat. HFpEF now accounts for more than half of patients with a clinical diagnosis of heart failure (HF) and its prevalence appears to be increasing. The growing number of younger patients afflicted with this condition seems to be driven largely by the epidemic of obesity and metabolic diseases.
The presence of significant knowledge gaps in this field and the dilemmas that clinicians face when evaluating and treating patients with HFpEF prompted us to organize the 2023 Charleston HFpEF Conference: The Latest Knowledge on Heart Failure with preserved Ejection Fraction. Our goal was to bring together a group of faculty experts who could help educate and update a wide scope of healthcare providers who are involved in management of these patients. As well, our hope was to raise awareness of ongoing trials testing new therapies for HFpEF and foster new professional connections for both clinical and research purposes. Finally, we sought to engage emerging cardiovascular healthcare providers to help them become involved in the crusade against HFpEF.
The conference agenda attempted to address some of the existing knowledge gaps in the HFpEF field. For example, there is a need for better standardization of the definition and diagnosis of HFpEF. Indeed, there is ongoing debate as to whether ejection fraction is the optimal way to categorize the type or phenotype of HF. If ejection fraction is used to subtype HF, the optimal cut-points for defining the various subcategories of HF are uncertain.
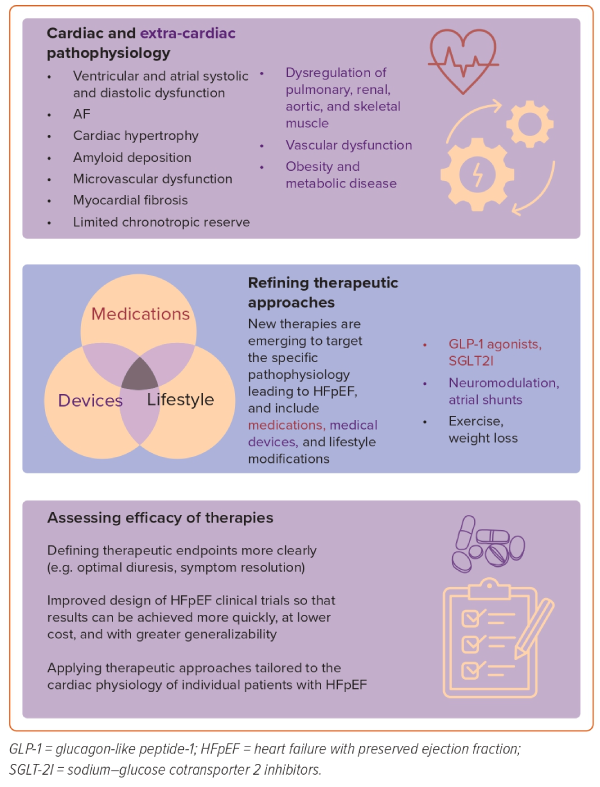
Another major push in the field is to better, or more specifically, identify and target the underlying abnormalities in patients with HFpEF, so that we can optimize therapeutic effects while minimizing toxicities and reduce costs. Despite the appeals of a targeted approach, it is still uncertain whether we should attempt to use a personalized or precision strategy that is more specific to individual patients or to focus on using all the potentially effective therapies in most patients. Along these lines, there are many different targetable pathophysiological processes that contribute to the syndrome of HFpEF. These include cardiac issues such as ventricular and atrial systolic and diastolic dysfunction, AF, cardiac hypertrophy, deposition of extracellular material such as amyloid protein, microvascular dysfunction, myocardial fibrosis, limited chronotropic reserve, and limited stroke volume or cardiac output reserve.
Abnormalities outside of the heart, including dysregulation of pulmonary, renal, aortic, skeletal muscle, and venous vascular function are all increasingly recognized to be important. Obesity and metabolic abnormalities clearly contribute to the rising prevalence of HFpEF, and they certainly play a role in the pathophysiology of the disease. Future studies may help to determine whether targeted or broad treatment strategies are the preferred approach.
In addition to understanding the complexities of the pathophysiological processes contributing to HFpEF, accurately confirming a diagnosis of HFpEF is also challenging. A variety of tools for diagnosing HFpEF exist, including imaging, biomarker measurement, tissue sampling, hemodynamic assessment at stress and rest, and the use of clinical scoring systems. At present there is no widely agreed upon method or even optimal cut-points for the various tests mentioned. The use of artificial intelligence may offer opportunities to incorporate many different pieces of data and to recognize patterns that are too complex for the human mind to identify.
Well-established therapies for HF, such as the use of loop diuretics to reduce fluid retention, are being re-examined with some surprising findings. At the same time, new and more effective treatments are rapidly emerging. We are finally seeing pharmacological agents that can improve symptoms and outcomes in HFpEF, including sodium–glucose cotransporter 2 inhibitors and glucagon-like peptide-1 agonists.
There is rapidly growing interest in device-based therapeutic approaches to HFpEF, such as atrial shunts. In addition, the field of neuromodulation is burgeoning. Targeting neural or humoral regulation of pulmonary, renal, splanchnic and systemic vasculature as well as neuro-cardiac reflexes is clearly gaining traction as a nonpharmacological way to attenuate the symptoms and the progression of the disease.
Data continue to emerge on the importance of exercise as a preventive and therapeutic approach in patients with HFpEF. Indeed, some consider HFpEF to be a disease of exercise deficiency. Optimal management of AF, a condition that may contribute to HFpEF while complicating the therapy, is an area of ongoing discussion.
Finally, there is a need for better design of HFpEF clinical trials so that results can be achieved more quickly and at lower cost. Ideally, trial results will be widely applicable to a broad population of HFpEF patients. Coming up with optimized enrollment and exclusion criteria as well as choosing the best, most clinically relevant and patient-centered trial endpoints remain challenging. The growing use of patient-reported outcomes is one such method of achieving these worthy goals.
We look forward to future meetings focusing on HFpEF so that we can continue fostering creative, collaborative, multidisciplinary approaches to many of the above issues (Figure 1).