Today, with the evolution of newer iterations of drug-eluting stents (DES), implantation techniques, intracoronary imaging, plaque modification tools, and adjunct pharmacological therapy, percutaneous coronary intervention (PCI) is offered to patients with complex coronary anatomy, left ventricular (LV) dysfunction, and/or multiple comorbidities. Although the volume of complex PCI continues to grow, the determinants of major adverse cardiovascular events (MACE), including the impact of gender on outcomes, remain unidentified. The purpose of this article is to review the current literature on outcomes of complex PCI as they apply to women. An important caveat of contemporary and historic evidence in this space, including randomized controlled trials (RCT), is the limited gender-specific analyses that explain notable differences between men and women undergoing complex PCI (Figure 1).
When addressing sex differences that pertain to biological sex at birth or other biological factors (including discussion of chromosomes, sex organs, and endogenous hormonal profiles), we have adopted the SAGER guidelines for sex and gender reporting. As such, we will designate sex differences with the terms ‘female’ and ‘male’. When addressing societal impact factors or in studies in which gender was self-reported, we will designate gender differences with the terms ‘women’ and ‘men’. We acknowledge there are data limitations in this review as many historic studies did not ask participants to specify biological sex and self-designated gender
Outcomes of PCI in Bifurcation Lesions
Approximately 15–20% of lesions encountered involve a bifurcation, defined as a coronary artery that continues as a larger main branch (MB) with a side branch (SB) that can be variable in size and angle from the MB.1 There are multiple approaches in the evaluation and treatment of bifurcation lesions, although they can be condensed into two main strategies: a stepwise provisional approach or upfront two-stent strategy. Factors impacting this decision include SB diameter and length and jeopardy of the myocardium for unanticipated compromise of SB flow and perceived ability to access through the MB struts.2 Women have consistently constituted a minority of patients studied in clinical trials, representing approximately 30% of patients in prospective and retrospective PCI studies.3,4 Regarding bifurcation PCI, retrospective analysis has shown that, compared with men, women tend to be older, with increased prevalence of serious comorbidities, such as diabetes, hypertension, peripheral artery disease, and chronic lung disease.5 Propensity score matching revealed increased major adverse events, driven by higher bleeding and transfusion rates, yet no difference in in-hospital mortality, vascular complications, or acute kidney injury between men and women.6,7
A large retrospective study within a single center examining complex PCI (5,004 of 20,419 patients), including bifurcation PCI, reported that women had more comorbidities, as described previously, and less complex coronary anatomy than men.6 Despite less complex anatomy, women had a significantly increased risk of MI at 1 year, with an HR of 1.63 (95% CI [1.12–2.38]) after adjustment for possible confounders.6 This observation is consistent and concerning, thus warranting studies designed to address both procedural techniques and outcomes in women specifically to better understand and mitigate the higher event rate.
Outcomes of LMS PCI
Historically, coronary artery bypass grafting (CABG) has been standard therapy in patients with left main stem (LMS) coronary artery disease (CAD). However, it has been suggested that PCI is an acceptable alternative, with guidelines recommending PCI in low- and intermediate-complexity CAD.2
A meta-analysis of long-term outcomes of PCI with DES versus CABG showed a comparable risk of all-cause death, MI, and cerebrovascular accident (CVA) between groups (HR 1.06; 95% CI [0.90–1.24]; p=0.48), with increased rates of repeat revascularization in the PCI group (HR 1.70; 95% CI [1.42–2.05]; p<0.001).8 Importantly, the population in that meta-analysis of the four main trials of PCI with DES versus CABG was predominantly men (76.7%).
There are important anatomical differences to be considered when comparing PCI versus CABG in males and females, particularly in the LMS. First, females tend to have smaller coronary arteries, which leads to the implantation of smaller stents and a smaller minimum stent area (MSA), which is associated with adverse outcomes in the LMS, including in-stent restenosis and stent thrombosis.9,10 Unfortunately, the uptake of intracoronary imaging to appropriately size the LMS during PCI in landmark randomized trials has been variable, ranging between 40% and 70%, only increasing the likelihood of undersizing in LMS PCI.8 Furthermore, clinical characteristics beyond the anatomical complexity have been shown to influence outcomes and need to be considered when selecting the most suitable revascularization strategy, such as diabetes, LV dysfunction, and chronic kidney disease.8
Randomized Trials of PCI versus CABG in LMS Coronary Artery Disease
There are no specific trials looking at PCI versus CABG in LMS disease in women; however, the four main trials (SYNTAX, EXCEL, NOBLE, PRECOMBAT) have reported gender-stratified outcomes.11–14
The SYNTAX trial compared PCI to CABG in patients with LMS CAD or three-vessel disease.15 At 5-year follow-up, major adverse cardiac and cerebrovascular events (MACCE; all-cause mortality, stroke, MI, and repeat revascularization) were significantly higher in the PCI than CABG arm, with sex an important driver of the mortality difference between groups (PCI arm: adjusted [a] HR for women 1.7, 95% CI [1.11–2.60]; CABG arm: aHR 0.59, 95% CI [0.332–1.10]).15 Four-year mortality data were assessed to determine independent correlates of mortality.10 After adjustment for age and SYNTAX score, female gender was an independent correlate of 4-year mortality in the PCI arm (HR 1.6; 95% CI [1.01–2.56]; p<0.048), leading to its inclusion in the SYNTAX II Score.11
The SYNTAXES (SYNTAX Extended Survival) study evaluated long-term survival in patients enrolled in the SYNTAX trial.16 At 10 years, women had a higher crude rate of all-cause mortality than men (32.8% versus 24.7%; log-rank p=0.002). However, after adjustment, female gender did not appear to be an independent predictor of all-cause mortality (aHR 1.02; 95% CI [0.76–1.36]; p=0.915). At 10 years, there was no difference in mortality rates between treatment arms in women (33.0% versus 32.5% for PCI versus CABG, respectively; log-rank p=0.600). The relative treatment effect of PCI versus CABG on mortality was not different between genders at 10 years (women: aHR 0.90, 95% CI [0.54–1.51], p=0.698; men: aHR 0.76, 95% CI [0.56–1.02], p=0.069; p for interaction=0.952).
The EXCEL trial compared PCI with everolimus-eluting stents to CABG in patients with unprotected LMS disease.12 The primary endpoint was a composite of death, MI, or cerebrovascular accident (CVA) at 3 years. Of the randomized patients, 23.1% (441/1,905) were women; compared with men, the women were older (mean [±SD] 67.1 ± 10.2 versus 65.6 ± 9.4 years; p=0.002) and more commonly presented with hypertension, hyperlipidemia, and diabetes. In addition, compared with men, women more frequently presented with congestive cardiac failure (10.5% versus 5.5%; p<0.001) and renal impairment (estimated glomerular filtration rate <60 ml/min/1.73 m2 27.2% versus 13.3%; p<0.001), but had lower anatomical complexity of disease (SYNTAX score 24.2 ± 9.0 versus 27.2 ± 9.3; p<0.001). Complete revascularization was more commonly achieved in women (37.4% versus 25.4%; p<0.001), with increased use of intravascular ultrasound (83.9% versus 75.1%; p=0.007), and women received lower numbers of arterial conduits than men (1.2 ± 0.5 versus 1.4 ± 0.6; p<0.001).15
Women experienced more complications than men in both the PCI (14.9% versus 8.9%; p=0.007) and CABG (13.2% versus 8.5%; p=0.04) arms.12 At 3 years, the rate of the primary endpoint (composite of all-cause death, MI, or CVA) among women was 19.7% and 14.6% in the PCI and CABG arms, respectively, compared with 13.8% and 14.7%, respectively, among men (p for interaction=0.06). The acute outcomes at 30 days were worse in women undergoing PCI, with a composite of all-cause death, MI, or CVA of 8.9%, compared with 6.2% in women treated with CABG. In men, the composite outcome was seen in 3.6% in those treated with PCI, compared with 9% in those treated with CABG (p<0.01). A significant interaction between gender and treatment was noted at 30 days in terms of the primary endpoint (p for interaction=0.003), but not at 3 years (p for interaction=0.06). In summary, in the EXCEL trial, women presented with increased clinical complexity but lower anatomical complexity and had an increased risk of ischemic and bleeding complications after PCI.12 Women undergoing PCI had a trend towards worse outcomes, with the highest numerical rate of the primary endpoint at 3 years; however, there were no significant interactions between gender and treatment for the 3-year endpoint.10
The NOBLE trial randomized patients with LMS disease to PCI or CABG.13 The primary endpoint was a composite of all-cause mortality, non-procedural MI, repeat revascularization, and stroke. Overall, 1,201 patients were included in the trial, with 1,184 in the 5-year follow-up, 22% of whom were women (n=256).13 Women presented more commonly with hypertension, diabetes, and statin treatment, but had overall lower anatomical complexity compared with men (SYNTAX score 21.3 ± 7.6 versus 22.7 ± 7.6 [p=0.009]; distal LMS lesion 75% versus 83% [p=0.01]).13 The 5-year PCI and CABG MACCE rates were 29% and 15%, respectively, in women and 28% and 20%, respectively, in men (log-rank p=0.001).13 The increased MACCE was driven by increased risk of non-procedural MI and repeat revascularization.
The PRECOMBAT trial randomized patients to PCI with sirolimus-eluting stents versus CABG, and the extended PRECOMBAT study followed patients for 10 years.14 Overall, 600 patients were enrolled, of whom 141 (23.5%) were women. There were fewer smokers among the women, but no other significant differences in clinical characteristics. Anatomical complexity was similar between women and men (SYNTAX score 24.7 ± 10.7 versus 24.8 ± 10.2, respectively; p=0.87).14 Complete revascularization rates were similar between genders and between revascularization techniques. The primary outcome was a composite of all-cause death, non-fatal MI, non-fatal stroke, and ischemia-driven target vessel revascularization (ID-TVR). The incidence of MACCE at 10 years was not significantly different between men and women in the overall population (27.3% versus 27.0%, respectively; p=0.713), in the PCI arm (30.6% versus 27.1%, respectively; p=0.853), or in the CABG arm (24.0% versus 26.9%, respectively; p=0.476).14
Registry Data
Given the inclusion and exclusion criteria of RCTs, as well as the small numbers of women included in RCTs, it is important to also consider registry data. The IRIS-MAIN Registry showed no difference in outcomes (death, MI, CVA) following PCI versus CABG between men (HR 0.92; 95% CI [0.72–1.17]) and women (HR 0.89; 95% CI [0.52–1.50]; p for interaction=0.65).17 In the DELTA Registry, women had a lower risk of the composite outcome of death, MI, and CVA with CABG than PCI (event rate 9.5% versus 15.3%; aHR 0.53; 95% CI [0.35–0.79]; p<0.001) and all-cause death (event rate 5.6% versus 11.7%; aHR 0.50; 95% CI [0.30–0.82]), with no significant differences seen in men.18 The MAIN-COMPARE Registry showed that at 10 years women had a lower incidence of death and serious adverse outcomes than men, with the risks of adverse outcomes varying by revascularization technique over time.19 In the short term (up to 1 year), compared with CABG, PCI had a lower risk for composite serious outcomes, namely death, MI, stroke, or repeat revascularization (aHR 0.41; 95% CI [0.19–0.91]; p=0.03). From 1 to 5 years, PCI had a higher risk for death (aHR 33.99; 95% CI [2.01–7.92]; p<0.001) and composite outcomes (aHR 2.93; 95% CI [1.59–5.39]; p=0.001). The 5- to 10-year risks were similar for PCI and CABG in women.19
Overall, the optimal revascularization modality for women with LMS CAD remains undetermined. Women appear to have a trend towards worse outcomes with PCI than CABG, but all trials have enrolled relatively small numbers of female patients. In both the EXCEL and NOBLE trials, women presented with increased cardiovascular risk factors, which may contribute to adverse longer-term outcomes.12,13 Female sex and a stent size of ≤3 mm independently conferred a smaller MSA of 5.3 mm2, which is associated with a higher 5-year incidence of target lesion revascularization.20 Given the association between smaller MSAs and adverse outcomes, it would appear imperative that stents are appropriately sized and optimized to achieve as large as possible an MSA, particularly in women.
Outcomes After Multivessel Revascularization
Similar to LMS, the outcomes following multivessel PCI remain worse in women than in their male counterparts. Kosmidou et al. reported that lesions in women had smaller reference vessel diameters and shorter lengths; these were core lab-adjudicated analyses.21 The unadjusted rate of MACE (18.9% versus 17.7%; p=0.003), all-cause death (10.4% versus 8.7%; p<0.001), cardiac death (4.9% versus 4.0%; p=0.003), and ID-TLR (10.9% versus 10.2%; p=0.02) was higher in women than in men.21 Multivariable analysis demonstrated that female gender was an independent predictor of MACE and ID-TLR only.21 As mentioned previously, studies such as the SYNTAX trial reported less complex CAD in women, which may be a selection bias because women are less likely to undergo coronary angiography and subsequent PCI owing to chronic kidney dysfunction, advanced age, or multiple risk factors and comorbidities. Yet Chichareon et al. evaluated over 15,000 patients in the GLOBAL LEADERS gender-specific subanalysis and found comparable rates of death and MI in men and women.22 However, it was notable that Chichareon et al. found that women experienced higher bleeding and hemorrhagic stroke events, which was not addressed by Kosmidou et al.21,22 Whether a lower uptake of radial access and body weight in women account for the higher bleeding events remains speculative. The limitation of the GLOBAL LEADERS trial is that more than 70% of patients had a single lesion.22
In the setting of both LMS and multivessel disease, we would be remiss not to mention the outcomes of CABG in women. A recent pooled analysis of four trials by Guadino et al. included over 13,000 patients.23 The authors noted that overall women had a significantly higher MACCE than men (95% CI [1.04–1.21]; p=0.004), but a similar mortality rate (95% CI [0.94–1.14]; p=0.51). The rate of MI and repeat revascularization, but not stroke, was higher in women than men. More interestingly, there were no significant differences in outcomes between men and women above the age of 75 years. As noted by the authors, these results can be explained, in part, by the large variations in baseline characteristics and suboptimal risk adjustment.23
Outcomes After Atherectomy for Calcified Coronary Stenoses
Calcific coronary lesions represent a particularly challenging PCI subset and are increasingly encountered in clinical practice. The presence of coronary artery calcium (CAC) is associated with a higher risk of stent malapposition and underexpansion, leading to an increased risk of intrastent restenosis and stent thrombosis.24 Despite the lower reported prevalence of CAC among women than men, female gender is an independent predictor of death, MI, stent thrombosis, and target lesion revascularization after PCI of calcified coronary lesions.6,25 Moderate to severe CAC was found in 25% of women undergoing PCI with DES in RCTs.26 This may be an underestimation of real-world rates due to the exclusion criteria of RCTs and the different methodologies used to assess CAC.26 Giustino et al. found that women undergoing PCI of calcified lesions with DES tend to have a worse clinical profile and remain at increased ischemic risk compared with men.26 However, the lower incidence of CAC in women, combined with the under-representation of women in RCTs investigating the safety and efficacy of cardiovascular devices, renders the assessment of the impact of CAC on women undergoing PCI a significant challenge.
Rotational Atherectomy
Rotational atherectomy (RA) has been used for over three decades in 0.8–3.1% of PCI procedures to treat complex calcified coronary lesions and achieve optimal lesion preparation before stent implantation.27
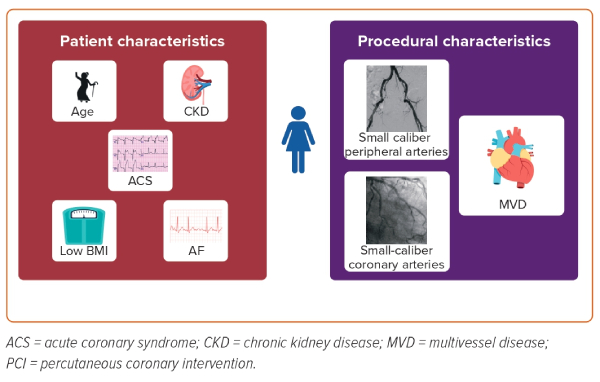
Women undergoing treatment with RA often present with more advanced CAD and smaller-caliber peripheral and coronary arteries.27–29 Observational registries investigating the utility of RA often report a higher-risk patient profile in women compared with men: women are usually older and present more often with acute coronary syndromes, chronic kidney disease, AF, a lower BMI, and worse lipid profiles than men.28,29 Both patient vulnerability and lesion complexity resulted in a higher rate of procedural net adverse cardiac events in women, predominantly driven by an excess of periprocedural bleeding and coronary events, including dissection and perforation leading to tamponade.28,30 Despite such results, women are still less likely to receive best practices, such as a radial approach to reduce bleeding and intravascular imaging to appropriately determine the burr, balloon, and stent size.30 For example, when the rate of intravascular imaging use exceeded 70% in RA registries, female gender was no longer associated with a higher incidence of periprocedural complications and MACCE.28 Notably, the higher periprocedural risk associated with RA use in women did not always translate into worse clinical outcomes, and conflicting results on long-term prognosis have been reported.28–30 Unfortunately, most of the studies evaluating gender differences in RA are retrospective registries, making it difficult to draw definitive conclusions. It is clear that more randomized trials investigating calcified coronary lesions and debulking techniques and devices in women are desperately needed.
Orbital Atherectomy
Similar to RA, there are limited data on orbital atherectomy (OA). ORBIT II was a non-randomized prospective multicenter single-arm study conducted in the US.31 The trial enrolled 443 patients (157 women). The women were older and had a lower mean estimated glomerular filtration rate than the men. The men were more likely to have had a previous CABG and to be smokers. Successful stent delivery and <50% residual stenosis were similar in both genders. In-hospital and 30-day MACE rates did not differ between the men and women.31
In 2016, Lee et al. reported low rates of MACCE in both women and men (0.7% versus 2.9%, respectively; p=0.14).32 There were no significant differences between women and men in the individual endpoints of death (0.7% versus 1.6%, respectively; p=0.43), MI (0.7% versus 1.3%, respectively; p=0.58), target vessel revascularization (0% versus 0%, respectively [none in either group]; p>0.99), and stroke (0.0% versus 0.3%, respectively; p=0.50), which were low in both groups.32 In addition, similar rates of angiographic complications were seen among women and men, including perforation (0.8% versus 0.7%, respectively; p>0.90), dissection (0.8% versus 1.1%, respectively; p=0.80), and no-reflow (0.8% versus 0.7%, respectively; p>0.90).32 Of note, that study was a small retrospective study that included a total of 458 consecutive real-world patients (only 144 of whom were women); it was not a randomized trial, and the results aligned with those reported in ORBIT II. However, the dissection rates reported by Lee et al. were similar between the two genders, which is very different from other trials noting a higher adjusted risk of severe dissections in women.32 It is difficult to make inferences given the limited data.
Intravascular Lithotripsy
Intravascular lithotripsy has emerged as a novel technology for plaque modification in recent years. The first gender-specific study of intravascular lithotripsy was published in 2022.33 The trial enrolled 628 patients, of whom 144 (22.9%) were women. The baseline characteristics of the patients in that trial were similar to studies on RA and OA, wherein women were older (p<0.001) and more likely to have hyperlipidemia (p=0.03), renal insufficiency (p=0.05), and prior MI (p=0.05).33 Women had a smaller mean reference vessel than in men (2.7 ± 0.4 versus 3.0 ± 0.5 mm; p<0.001), as well as a shorter lesion length (22.4 ± 10.3 versus 25.0 ± 11.7 mm; p=0.01) and less SB involvement (22.9% versus 32.4%; p=0.03).33 There were no significant differences between women and men in the primary safety endpoint (8.3% versus 7.1%, respectively; p=0.61) or the primary efficacy endpoint (91.7% versus 92.6%, respectively; p=0.72).33 The rate of complications, including flow-limiting dissection, perforation, abrupt closure, slow flow, and no reflow, were similar for women and men (1.6% versus 2.3%, respectively; p=0.75).33
There are many tools currently available for debulking, such as cutting balloons, laser atherectomy, and other directional atherectomy devices. Collectively, little evidence describing outcomes is available for these technologies.
Outcomes in Cardiac Arrest and Cardiogenic Shock
There are few data in RCTs evaluating differences in the treatment of men and women for cardiac arrest and cardiogenic shock (CGS) due to atherosclerotic CAD and acute MI (AMI). Most data are retrospective. Using data from the National Inpatient Sample (NIS) from US hospitalizations (2006–15), in-hospital mortality for ST-elevation MI (STEMI) and CGS was higher for women (40–45%) than men (30–34%).4,5 With respect to racial and ethnic disparities, Hispanic women had the highest odds of in-patient mortality (aOR 1.46; 95% CI [1.26–1.70]; p<0.001).4 Another analysis of the NIS hospitalizations from 2000 to 2017 revealed that women receive less coronary angiography and PCI, and, unfortunately, had higher in-patient mortality (52.6% versus 40.6% in men) after presenting with cardiac arrest and AMI.34 Similar results have been observed in Europe: a study from Spain evaluating CGS-AMI patients from 2003 to 2015 found adjusted mortality was higher in women than in men over time (65.8% versus 58.1% most recently), and that female gender was an independent predictor of mortality (OR 1.18; 95% CI [1.10–1.27]; p<0.001).35 Regarding multivessel CAD and CGS with PCI, there are no studies evaluating outcomes in men versus women. Data suggest that there is harm in multivessel PCI in those patients with CGS and AMI.36
Outcomes in Women With Concomitant Structural Heart Disease
CAD is a common diagnosis among patients undergoing transcatheter aortic valve replacement (TAVR). The timing of PCI in such settings remains controversial. Few studies have captured outcomes in men and women undergoing PCI along with structural interventions, such as TAVR. Moreover, outcomes of patients undergoing TAVR and PCI for significant CAD have yielded conflicting results.37 An early study from Griese et al. in 2014 enrolled 64% women, with the investigators noting that all those undergoing TAVR plus PCI had worse outcomes.37 The mean logistic European System for Cardiac Operative Risk Evaluation (EuroSCORE) was 21.7% for the TAVR plus PCI group and 20.3% for the TAVR alone group (p=0.47). The incidence of MI and 30-day mortality was higher in the TAVR plus PCI group (6% versus 1% [p=0.01] and 15% versus 5% [p=0.01], respectively). Both a synchronous (18%) versus staged (15%) strategy for PCI had a comparable early mortality rate (p=1.0). The 2-year survival was worse in the TAVR plus PCI group (p=0.03), with an OR of 1.66 (p=0.04).
Wenawesar et al. reported prospective data from the Bern TAVI registry.38 In patients with CAD, myocardium at risk was assessed using the Duke myocardial jeopardy score. In the Bern TAVI registry, 167 patients had CAD and 59 underwent either staged (n=23) or concomitant (n=36) PCI. Women represented >50% of the studied cohort. Clinical outcomes at 30 days was similar for patients undergoing isolated transcatheter aortic valve implantation (TAVI) compared with TAVI combined with PCI in terms of death (5.6% versus 10.2%; p=0.24), major stroke (4.1% versus 3.4%; p=1.00), and the Valve Academic Research Consortium (VARC)-defined combined safety endpoint (31.0% versus 23.7%; p=0.33).38 Similarly, in the study of Abdel-Wahab et al., the rates of 30-day stroke, major bleeding, major vascular complications, and VARC-defined combined safety endpoint did not differ between the TAVI and TAVI plus PCI groups (11% versus 13%, respectively; p=0.74).39
Ghrair et al. compared in-hospital periprocedural outcomes of combined TAVR and PCI during the same index hospitalization versus the isolated TAVR procedure in a retrospective observational study.40 The investigators enrolled 852 patients from the Nationwide Readmissions Data in 2016. The mean patient age was 80.5 years and women constituted 45.9% of the population. TAVR–PCI was associated with higher in-hospital all-cause mortality (4.5% versus 1.7%; p<0.01), a longer length of stay (10.5 versus 5.4 days; p<0.01), and a higher incidence of CGS (9.4% versus 2.1%; p<0.01), the use of mechanical circulatory support devices (6.8% versus 0.7%; p<0.01), mechanical complications of the prosthetic valve (6.8% versus 0.7%; p<0.01), pulmonary vein isolation (0.9% versus 0.4%; p=0.01), acute kidney injury (25.5% versus 11.5%; p<0.01), and bleeding (25.2% versus 18.1%; p<0.01) compared with isolated TAVR.40 There was no subanalysis examining gender-specific outcomes in any of these studies; most were not prespecified or powered to provide definitive conclusions.38–40
The most relevant randomized trial in this group is the ACTIVATION trial.41 This study enrolled 235 patients who underwent randomization. At 1 year, the primary composite endpoint occurred in 48 (41.5%) patients in the PCI arm and in 47 (44.0%) patients in the no-PCI arm. The requirement for non-inferiority was not met (difference: −2.5%; one-sided upper 95% CL: 8.5%; one-sided non-inferiority test p=0.067).41 On analysis of the as-treated population, the difference was −3.7% (one-sided upper 95% CL: 7.5%; p=0.050). Mortality was 16 (13.4%) in the PCI arm and 14 (12.1%) in the no-PCI arm.41 At 1 year, there was no evidence of a difference in the rates of stroke, MI, or acute kidney injury, with higher rates of any bleed in the PCI arm (p=0.021).41 Women constituted 48% of the total and the study was not powered to provide gender-specific outcomes.
Registries such as the WIN TAVI registry did not specifically evaluate revascularization and no conclusions can be drawn at this time.42 However, it is notable that prior coronary revascularization was an independent predictor of 1-year death or stroke (HR 1.50; 95% CI [1.03–2.19]; p=0.035).
Conclusion
Revascularization success, particularly in complex PCI cases, is contingent upon many factors, including the complex interplay of differences in sex-based comorbidities and biological factors, the propensity for bleeding complications, and outpatient follow-up. It is reassuring that the new American College of Cardiology/American Heart Association/ Society of Cardiovascular Angiography and Interventions consensus guidelines on coronary artery revascularization emphasize treatment on clinical indications, regardless of sex/gender or race/ethnicity, towards greater efforts to reduce disparities of care.43 However, when evaluating the body of evidence for complex PCI, it becomes abundantly clear that there are gaps in published data that can guide clinical practice. This is an opportune time to seek gender-specific trial data as new technologies and devices emerge. 










