Introduction: Assessment of congestion in heart failure (HF) is challenging. Different biomarkers of congestion have been used in clinical practice, but their correlations with blood volume analysis (BVA) measurements are not well characterized. Furthermore, whether the association differs across left ventricular ejection fraction (LVEF) subgroups is not known.
Methods: We enrolled patients with HF who underwent BVA and had same-day measurements of N-terminal pro B-type natriuretic peptide (NT-proBNP), carbohydrate antigen 125 (CA125), and serum sodium. BVA was performed using the I131-albumin indicator dilution technique. Absolute values and percent deviation from ideal values of total blood volume (TBV) and plasma volume (PV) were reported. The correlation between each biomarker and TBV/PV%deviation was determined using Pearson’s correlation. Patients were categorized into two groups using an LVEF cut-off of 50%. The same analysis was repeated by LVEF subgroups.
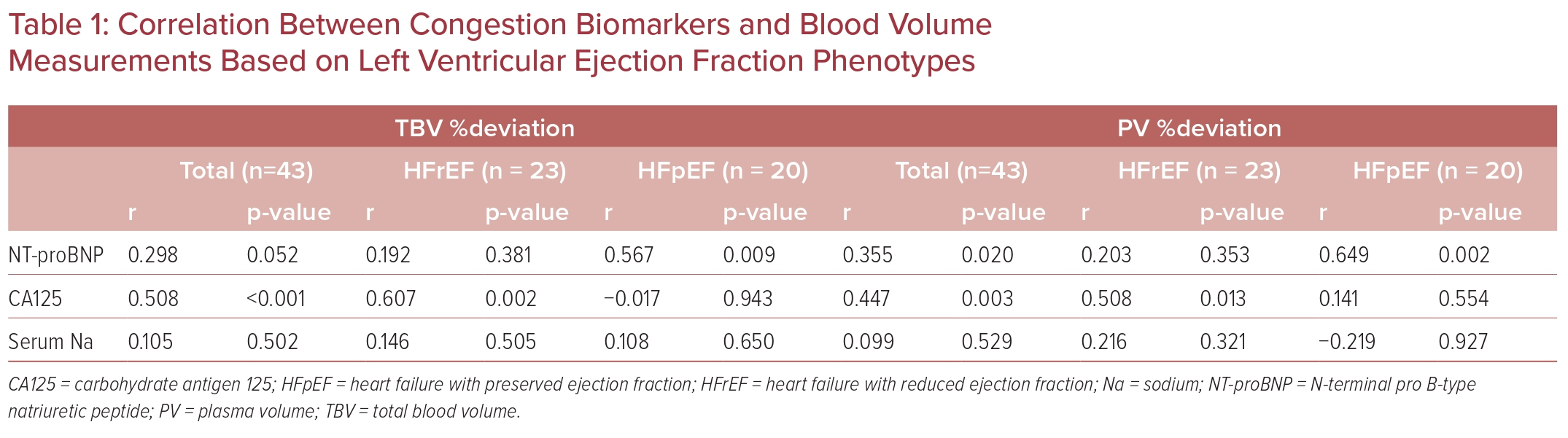
Results: Overall, 43 patients (61 years, 35% female, 37% black, 47% HF with preserved ejection fraction [HFpEF]) were included. There was no difference in age, sex, comorbidities, or biomarker levels between LVEF subgroups. CA125 was correlated with TBV%deviation (r=0.508) and PV%deviation (r=0.447; Table 1). NT-proBNP was only correlated with PV%deviation (r=0.355). Serum sodium was not correlated with any BVA measurements. The correlation between CA125 and BVA measurements was only observed in HF with reduced ejection fraction (TBV: r=0.607, PV: r=0.508). In contrast, there was a correlation between NT-proBNP and BVA measurements only in HFpEF (TBV: r = 0.567, PV: r = 0.649).
Conclusion: Correlation between congestion biomarkers and BVA measurements exists but differs between LVEF subgroups. Further studies are warranted to explore the underlying mechanisms of these observations. 









