Introduction: Heart failure with preserved ejection fraction (HFpEF) is a clinical syndrome that is defined by the presence of signs and symptoms of heart failure in the setting of preserved left ventricular systolic function. There is a differential for HFpEF syndromes, and recognition of HFpEF mimics is essential. We present a case of idiopathic pericardial disease mimicking HFpEF.
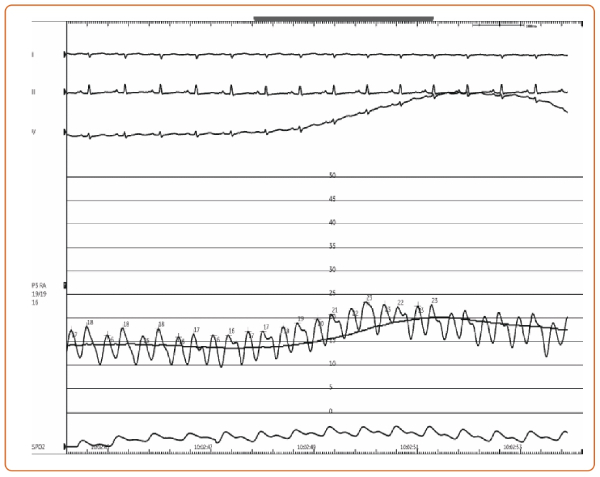
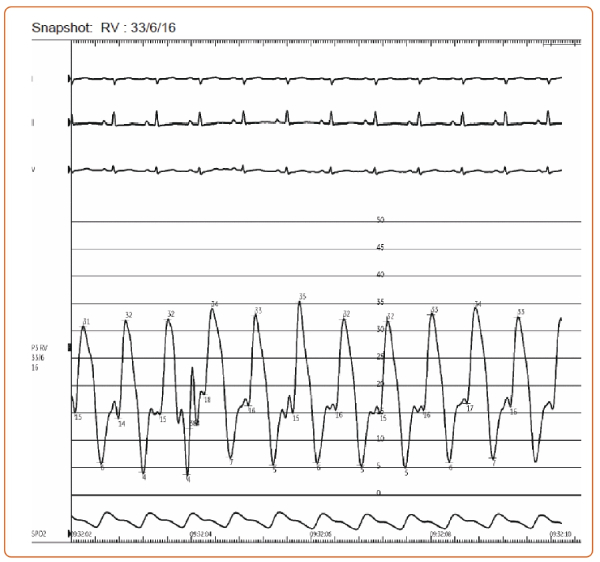
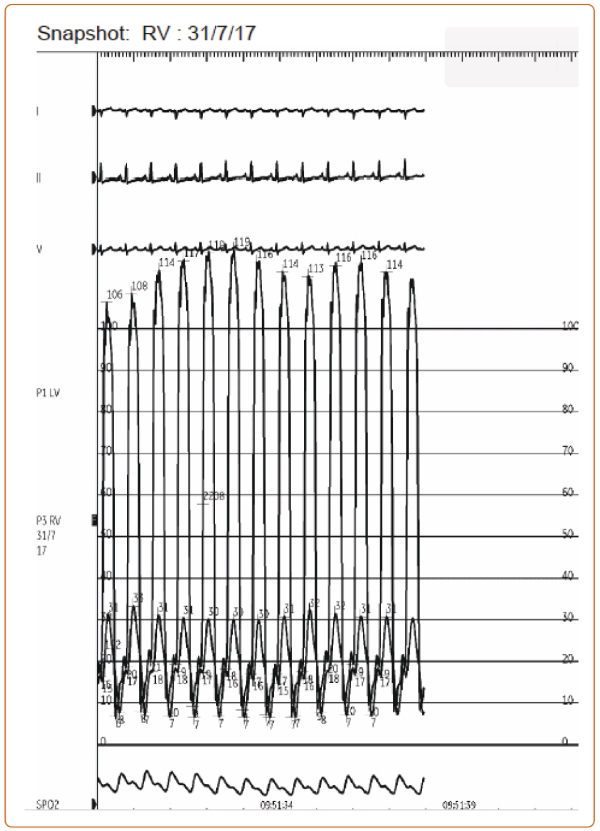
Case: A 64-year-old man without past medical history was referred to our heart failure program for chronic dyspnea. Six months prior, coronary calcium CT obtained for risk stratification revealed incidental pericardial thickening on the background of chronic pericardial calcifications. Vital signs were within normal limits. Physical examination was notable for elevated jugular venous pressure (7 mm) and a positive Kussmaul’s sign. Electrocardiogram showed normal sinus rhythm, right axis deviation, possible right ventricular hypertrophy, and abnormal QRS-T angle. An initial echocardiogram showed inferior and inferoseptal apical hypokinesis, septal bounce, normal left atrial size, a lateral E’ 10, and septal E’ 9, E/E’ ratio of 6. Labs were notable for elevated total bilirubin (1.6 mg/dL). Cardiac catheterization showed findings consistent with constrictive physiology including positive Kussmaul (Figure 1) and square root (Figure 2) signs, elevated biventricular filling pressures, and ventricular interdependence following volume loading (Figure 3).
Discussion: There are various cardiac and noncardiac pathologies that mimic HFpEF. In general, the differential diagnosis for HFpEF is broad, and a high index of suspicion coupled with appropriate diagnostic testing is required to establish the diagnosis and rule out HFPEF mimics. More recently, the H2FPEF risk calculator has proven a useful tool to determine the pretest probability of HFpEF and guide subsequent cardiac testing.
Our patient had a low H2FPEF score of 1, suggesting a low likelihood of traditional HFpEF. However, given clinical concern, additional cardiac testing was obtained to better determine his hemodynamics invasively. In this case, the patient underwent simultaneous right- and left heart catheterization, which revealed constrictive physiology. Pericardial enhancement and thickening was also seen on cardiac MRI, leading to a diagnosis of pericardial constriction, in this case idiopathic.
The pericardium exerts significant modulatory effects on ventricular hemodynamics, which results in impaired diastolic filling and ventricular pressure equalization despite preserved ventricular function on echocardiography. This physiology may clinically present as HFpEF but is treated differently; it is a potentially curable form of heart failure. Therefore, the evaluation of HFpEF should include probability testing and – if clinical suspicion remains – more advanced imaging and hemodynamic tests.
Conclusion: HFpEF should be considered as a cause of unexplained dyspnea particularly in the presence of typical risk factors. Consideration of HFpEF mimics is essential in all cases of HFpEF, but particularly when patient comorbidities do not reflect those of typical HFpEF.