Due to increasing life expectancy and age being a significant factor in the development of coronary artery disease (CAD), people >65 years now constitute the majority of patients presenting with acute coronary syndromes (ACS). In the US more than 780,000 patients experience an ACS event each year, of whom 70% have non-ST-elevation MI (NSTEMI).1 About 60–65% of MI occurs in patients ≥65 years and 28–33% in patients ≥75 years of age.2 Furthermore, 80% of deaths related to MI occur in patients ≥65 years of age. Despite these numbers, elderly patients, particularly those aged ≥75 years have been underrepresented in ACS trials.
The management of ACS in the elderly can be challenging because they frequently present with atypical symptoms that delay diagnosis, pre-existing multiple comorbidities, frailty, and increased risk of complications.3 Though an early invasive approach in high-risk ACS can result in a significant improvement in cardiovascular outcomes, elderly patients are often treated conservatively with medical management due to local physician practices, a dearth of evidence from randomized controlled trials (RCTs), and a lack of age-specific guidelines.4–7 Management decisions are therefore usually based on physician judgment and patient preference with significant consideration given to quality of life, risks and benefits of an invasive approach, life expectancy, and cognitive and functional status. In this review, we discuss the characteristics of elderly patients presenting with ACS, specific geriatric conditions that need to be considered while making treatment decisions in these situations, and available evidence, guidelines, and future directions for invasive management of elderly patients with ACS.
Characteristics of Elderly Patients with Acute Coronary Syndrome
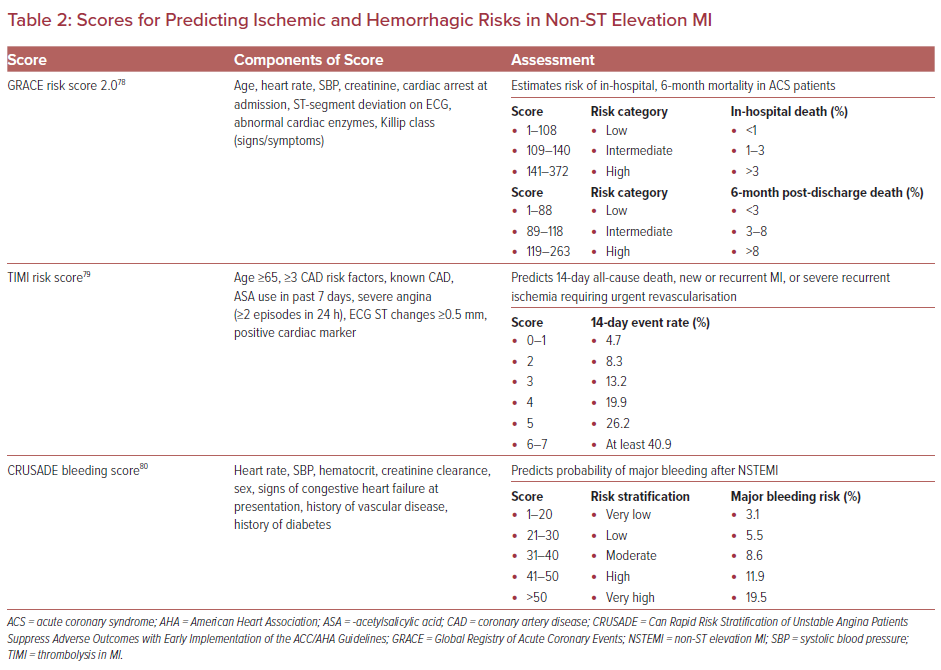
Age predisposes to the development of CAD due to various biological and functional changes, including increased oxidative stress, apoptosis, inflammation, and genomic instability that contribute to increased vascular stiffness, endothelial dysfunction, and thrombogenicity.3,8 Moreover, several established risk factors for CAD, including hypertension, hyperlipidemia, diabetes, and renal dysfunction are common in elderly patients (Table 1) leading to ACS being more common in this age group.3
The diagnosis and management of ACS in elderly patients is often challenging due to atypical presentation, polypharmacy, comorbidities, cognitive and functional status, and socio-economic factors.3,9 Atypical chest pain and dyspnea are common, while syncope, fatigue and confusion are less frequent presenting symptoms among elderly patients with ACS. Elderly patients who take multiple medications are prone to an increased risk of adverse drug interactions, and hence it is important to balance risks of polypharmacy with the benefit of taking guideline-directed medications proven to be of benefit in the elderly.10 Multiple comorbidities commonly seen in elderly patients, such as chronic kidney disease (CKD), peripheral arterial disease (PAD), dementia, heart failure (HF) or MI have a negative prognostic effect in patients with ACS.11 Diminished organ reserves and altered cognitive and functional status influence disease presentation, treatment, and recovery.12 In addition, older people living in impoverished and rural areas are more likely to have a delayed presentation, and may be farther away from medical facilities which delays timely care.13
There are several other important factors related to older age that need to be considered in patients presenting with ACS. Frailty, a state of diminished physiological reserve and increased vulnerability for poor resolution of homeostasis after a stressor event is seen more often in the elderly.14 In the US, prevalence of frailty ranges from 4–16% in men and women ≥65 years of age.15,16 In the 90+ study by Lee et al., prevalence of frailty was 24% and 39.5% among those aged 90–94 years and ≥95 years, respectively.17 Frailty is associated with increased risk of procedural complications, falls, disability, and is a strong independent predictor of 1-year mortality in elderly patients with ACS.18 A meta-analysis of 15 studies showed that frailty in elderly ACS patients increased the risk of all-cause mortality, any-type of cardiovascular disease, major bleeding and hospital readmissions by 2.65, 1.54, 1.51 and 1.51-fold, respectively.19 Several studies involving elderly ACS patients undergoing percutaneous coronary intervention (PCI) showed frailty to be associated with worse outcomes following the intervention.20–24 Thus, the assessment of frailty in elderly patients with ACS is essential to help physicians appraise the comprehensive prognostic risk of implementing appropriate management strategies.
Nutritional status is another important consideration in the elderly since malnutrition adversely affects the prognosis of elderly patients and is often unrecognized and therefore untreated.25 A multi-center study showed that around 71% of hospitalized older patients are at nutritional risk or are malnourished which is associated with increased mortality.26 Another study classified 908 older patients hospitalized with ACS (mean age 82 ± 6 years) into malnutrition (4%), at high-risk of malnutrition (40%) and normal nutrition (56%) using the Mini Nutritional Assessment-Short Form (MNA-SF) score. During a 288-day follow-up period, 31%, 19% and 3% mortality rates were seen in malnourished subjects, at-risk patients and in patients with a normal nutritional status, respectively (p<0.001). MNA-SF was found to be an independent predictor of all-cause mortality (HR 0.76; 95% CI [0.68–0.84]) in elderly ACS patients.27 As such, it is important that targeted nutritional interventions and rehabilitation programs that may improve the outcome in elderly patients with ACS be investigated in clinical trials and appropriate consideration be given to nutritional status while making decisions about management.
Delirium, characterized by acute decline in attention and cognitive dysfunction, is a frequent complication during hospitalization in elderly patients associated with poor clinical outcomes and increased mortality.28 The incidence of delirium is reported to be 17.2% in patients ≥75 years admitted for acute cardiac diseases.29 Another study including 527 octogenarians with NSTEMI had a 7% incidence of delirium during hospitalization. The study also found delirium to be independently associated with mortality (HR 1.47, 95% CI [1.02–2.13]; p=0.04) and bleeding events (OR 2.87; 95% CI [1.98–4.16]; p<0.01) at 6 months.30 Thus, effective measures to prevent delirium, such as frequent orientation, cognitive stimulation, environmental modification and non-pharmacological sleep aids, early mobilization, visual and hearing aids, and avoiding medications precipitating delirium, especially benzodiazepines should be implemented in hospitalized elderly patients with ACS.31
Contrast-induced nephropathy (CIN), a form of acute kidney injury that occurs shortly after administration of iodinated contrast, is prevalent in elderly patients. Among at-risk patients, especially those with diabetes and CKD, the risk following coronary angiography with or without intervention is reported to be 10–30%. For all at-risk patients, preventive measures including use of low-osmolar or iso-osmolar contrast media with lower doses, hydration with 1 ml/kg/h of isotonic saline 6–12 hours pre-procedure, intra-procedure, and 6–12 hours post-procedure may be implemented.32,33
Finally, elderly patients with ACS are more likely to present with NSTEMI compared with ST-elevation MI (STEMI) and have higher rates of type 2 MI due to myocardial oxygen supply and demand mismatch. They are at increased risk of thrombotic, bleeding and PCI complications, and the rate of successful revascularization is lower due to more complex coronary disease.34 Given the high risk of bleeding complications, these patients need a carefully chosen anti-thrombotic with dose adjustment based on body weight and renal function.
ST-elevation MI
Studies have shown that 30% of patients admitted with STEMI are 75 years or older.2 There is an annual increase of >160,000 octogenarians in the US, and the trend is estimated to increase by fivefold by 2040.35 Thus, the proportion of elderly patients with STEMI is also expected to increase over time. STEMI care in the elderly can often be challenging and delayed due to longer symptom onset to first medical contact, atypical symptoms, and ECG findings of STEMI being masked by pre-existing ECG changes, such as baseline left ventricular hypertrophy, changes from prior MI, conduction system disease with bundle branch block, or AF.2,36
Despite these challenges and high acuity, studies show elderly STEMI patients, including the very elderly ≥85 years, have reasonable long-term survival and excellent quality of life when treated aggressively with reperfusion therapy.37 Even patients >90 years treated with primary PCI have two- to threefold lower rate of inhospital and 12-month mortality compared with those treated medically.5,6 Early revascularization in elderly patients had an adjusted survival benefit as compared to delayed or no revascularization in the non-randomized SHOCK registry.38 Primary PCI is also superior to fibrinolysis, with the TRIANA trial demonstrating that PCI was superior to fibrinolysis (OR 0.64; 95% CI [0.45–0.91]) in reducing the composite of all-cause mortality, re-infarction or stroke at 30 days.2,39 When primary PCI is not readily available, the patient should be treated with thrombolysis, as supported by the STREAM trial.40 Thus, in elderly patients with STEMI, primary PCI is the preferred reperfusion strategy regardless of age, with fibrinolysis reserved for those patients where primary PCI is not immediately available. This recommendation is in accordance with 2013 American College of Cardiology (ACC)/American Heart Association (AHA) and 2017 European Society of Cardiology (ESC) guidelines (level of evidence A).41,42 Despite this benefit, elderly patients who are frail or have comorbidities, such as CKD, are often managed medically, leading to an increased risk of mortality.43
Elderly patients presenting with STEMI are more likely to have multivessel coronary disease compared to younger patients.44 The COMPLETE trial showed that multivessel PCI was superior to culprit-only PCI in reducing the risk of the composite of cardiovascular death, ischemia-driven revascularization, or MI in STEMI patients. However, these results cannot be generalized to elderly patients as a whole since the average age of patients enrolled in the COMPLETE trial was 62 years with <40% of patients being >65 years.45 A sub-study of DANAMI-3-PRIMULTI trial and a few other studies demonstrated no significant benefit to prophylactic complete revascularization of non-culprit lesions in elderly STEMI patients after treatment of the culprit lesion.46–48 Further RCTs including elderly patients are needed to understand the best management plan in elderly patients with STEMI and multivessel CAD.
Non-ST-elevation MI
The majority of patients admitted with NSTEMI are ≥70 years.49 The United Nations has projected that the proportion of the global population aged ≥80 years will triple over the next 20 years, and thus the proportion of elderly patients presenting with NSTEMI is expected to increase.50
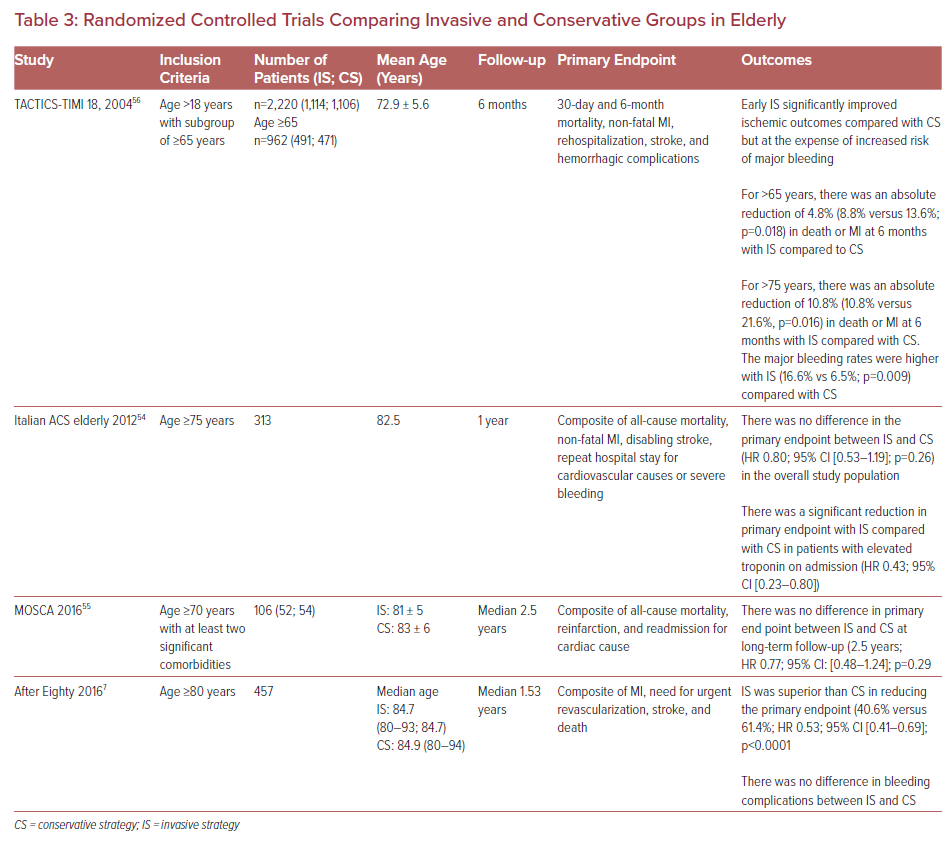
The management of NSTEMI in elderly patients is based on the individual assessment of ischemic and bleeding risk. Age is an independent risk factor for both thrombotic and bleeding events in the setting of ACS.36 Several prognostic scores have been developed to predict the ischemic and hemorrhagic risks in patients with NSTEMI (Table 2). Risk stratification using these scores helps to make appropriate invasive or conservative management decisions. The Global Registry of Acute Coronary Events (GRACE) score has been validated to estimate the risk and survival in the acute phase of ACS in nonagenarians.51 The Thrombolysis in MI (TIMI) risk score was shown to be a robust predictor of both in-hospital and post-discharge mortality in elderly women in a study by Furnaz et al.52 The predictive performance of the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines (CRUSADE) bleeding score is less accurate in elderly patients than younger patients with ACS.53
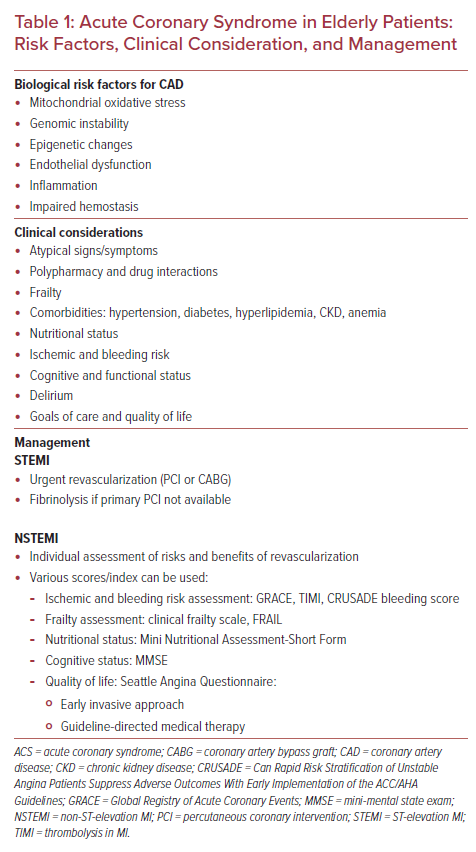
There are several RCTs that compare outcomes between invasive and conservative approaches for ACS in the elderly population (Table 3). An Italian ACS study including patients ≥75 years with NSTEMI found no significant benefit of an early aggressive approach within 72 hours as compared to an initial conservative strategy in reducing the composite primary endpoint of death, MI, stroke, and repeat hospital stay for cardiovascular causes or severe bleeding within 1 year. However, in subgroup analysis, patients with elevated troponin levels had a lower primary endpoint from early invasive strategy (HR 0.43; 95% CI [0.23–0.80]).54 The MOSCA trial is the first RCT which compared the outcomes of routine invasive versus conservative strategy in NSTEMI patients ≥70 years with at least two comorbidities (PAD, cerebral vascular disease, dementia, chronic pulmonary disease, CKD, or anemia). It reported that invasive management did not modify long-term outcomes (all-cause mortality, reinfarction and readmission for cardiac cause) during the 2.5-year follow-up in elderly patients compared to a conservative approach (coronary angiogram only if recurrent ischemia or HF). However, an invasive approach had better short-term outcomes at 3 months in terms of mortality (HR 0.348; 95% CI [0.122–0.991]; p=0.048), and mortality or ischemic events (HR 0.432, 95% CI [0.190–0.984]; p=0.046).55 The TACTICS-TIMI 18 trial found that early invasive strategy within 4 to 48 hours had better outcomes as compared to conservative management with an absolute reduction of 4.8% in death or MI at 6 months among NSTEMI patients >65 years and absolute reduction of 10.8% among patients >75 years. But major bleeding rates were higher with an invasive approach in patients >75 years (16.6% versus 6.5%; p=0.009).56
The After Eighty study including NSTEMI patients ≥80 years showed that an invasive approach was superior to a conservative strategy in reducing rates of MI, urgent revascularization, stroke, and death (40.6% versus 61.4%; HR 0.53; 95% CI [0.41–0.69]), with no significant difference in the rates of major and minor bleeding during a median of 1.53 years follow-up.7 Similar results were seen in the SENIOR-NSTEMI trial that estimated mortality in a non-randomized, propensity-matched analysis in NSTEMI patients ≥80 years. The adjusted cumulative 5-year mortality was 36% in patients receiving invasive management within 3 days of peak troponin as compared to 55% in patients with a non-invasive approach (adjusted HR 0.68; 95% CI [0.55–0.84]).57 The SENIOR-RITA (NCT03052036) is an ongoing multicenter, open-label randomized trial comparing invasive and conservative strategies and the time to cardiovascular death or non-fatal MI within 1 year in type 1 NSTEMI patients ≥75 years. Overall, these RCTs included a very selective population, limiting the generalization of these results to the entire elderly population. Moreover, some of these trials studied the elderly population as the subgroup of a larger cohort and hence analysis may be underpowered for certain endpoint comparisons.
A meta-analysis of six trials by Reano et al. compared the effectiveness of an early invasive strategy within 48–72 hours to a conservative approach in NSTEMI patients ≥65 years. Of a total of 3,768 patients, 1,986 were assigned to the invasive strategy and 1,782 to the conservative treatment group. The invasive strategy was defined as intervention either by PCI or coronary artery bypass graft within 48–72 hours of initial evaluation. The results showed a significant reduction in the need for revascularization during an average follow-up period of 2 years in the invasive group (2%) compared to the conservative treatment group (8%; RR 0.29; 95% CI [0.14–0.59]). However, there was no significant difference in the rate of all-cause mortality, cardiovascular mortality, stroke, and MI between the two groups with significant heterogeneity. The small number of events and sample sizes in addition to the different age cut-offs and different follow-up periods in the included studies may have been the sources of heterogeneity for death and MI outcomes.58
Another meta-analysis involving 13 studies (four RCTs and nine observational studies) by Ma et al. including a total of 832,007 elderly NSTEMI patients >75 years showed a significant decrease in the risk of death at follow-up from 6 months to 5 years in patients treated with an invasive approach compared to conservative treatment (RR 0.65; 95% CI [0.59–0.73]; p<0.001). This was mostly seen in observational studies. However, there was a significant increase in bleeding risk in hospital patients treated with invasive strategy compared to conservative approach but no difference in major bleeding was observed between the two groups (RR 1.78; 95% CI [0.31–10.13]; p=0.514).59 In a meta-analysis of eight trials including 5,324 patients, overall, there was no significant mortality reduction in the early invasive group compared with the delayed invasive group. However, lower mortality was found with the early invasive strategy in some high-risk patients including patients with elevated cardiac biomarkers at baseline (risk reduction 24%), diabetes (risk reduction 33%), GRACE risk score >140 (risk reduction 30%), and those aged ≥75 years (risk reduction 35%).4 Based on available data, we recommend an early invasive approach in elderly patients with high-risk NSTEMI, considering the individual risks and benefits of revascularization in accordance with the 2014 AHA/ACC (level of evidence A) and 2020 ESC guidelines (level of evidence B).1,60
Special Considerations During Invasive Management of Elderly Patients with Acute Coronary Syndrome
There are several important things to consider for elderly patients undergoing PCI for ACS (Table 4). First, elderly patients with ACS have an increased risk of bleeding with use of anti-thrombotic therapies from the PCI access site, and are at risk of hemorrhagic stroke from fibrinolysis.2 On the other hand, under-prescription of appropriate anti-thrombotic agents in elderly patients increases the risk of ischemic events. Though not specific to the elderly, the Predicting Bleeding Complications in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score can be used to predict the risk of bleeding in ACS patients on dual antiplatelet therapy (DAPT) post-PCI.61 A more conservative approach is recommended for patients who score ≥25. A study by Guerrero et al. showed that elderly patients ≥75 years have PRECISE-DAPT values above the cut-off point for high bleeding risk and recommend using different cut-off values for them.62 A shorter duration of 3–6 months instead of 12 months DAPT may be considered for elderly patients at high risk of bleeding post-PCI with newer generation drug-eluting stents (DES). For patients requiring oral anticoagulation (OAC) post-PCI, a P2Y12 inhibitor with OAC should be used without aspirin to reduce the risk of bleeding.63 The right choice of P2Y12 inhibitor in elderly patients post-PCI is important to maximize ischemic benefit and reduce bleeding risk. Prasugrel must be avoided in elderly patients ≥75 years with ACS undergoing PCI due to the increased risk of bleeding, as seen in the TRITON TIMI 38 trial.64
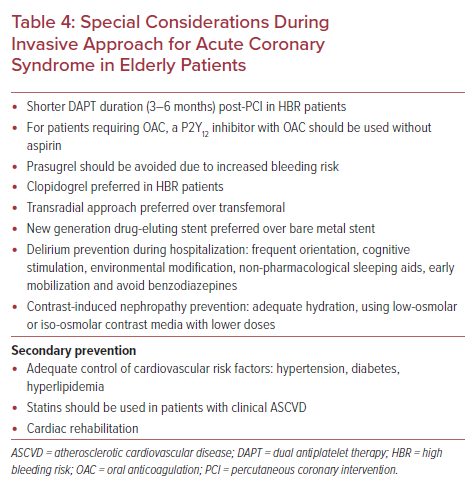
The Elderly ACS 2 trial, which aimed to demonstrate superiority of low-dose prasugrel (5 mg) over clopidogrel (75 mg) in elderly patients with ACS, was prematurely interrupted because of futility for efficacy.65 Although, in the PLATO trial, the net clinical benefit favored the use of ticagrelor over clopidogrel even in the elderly despite increased bleeding risk, elderly patients ≥75 years with ACS constituted only 15% of the overall ACS trial population.66 Moreover, it is possible that patients with lower bleeding risk may have been included in the trial and hence overall net clinical benefit of ticagrelor compared with clopidogrel in elderly patients is not well defined. The POPular AGE trial showed that in patients ≥70 years with NSTEMI, clopidogrel is a favorable alternative to ticagrelor, especially where there is a high bleeding risk, because of reduced bleeding events without an increase in the combined endpoint of all-cause death, MI, stroke, and bleeding.67 Thus, clopidogrel may be the P2Y12 of choice in elderly patients with ACS at high bleeding risk.
Second, although there is increased usage of the transradial approach (TRA) for PCI, its adoption is lowest in elderly patients despite similar reductions in mortality and major adverse cardiac and cerebrovascular events outcomes (MACCE) associated with TRA use compared with younger patients.68 A meta-analysis of 17 studies showed decreased risk of stroke, vascular complications, and mortality benefit with TRA for PCI in elderly patients with STEMI.69 Although the access site crossover rate is higher in elderly people with TRA compared with the transfemoral approach (TFA), mainly due to an increased level of vascular calcification and arterial tortuosity, its use remains acceptably low considering the advantages associated with TRA.70 Given reduced bleeding and mortality with TRA compared with TFA, it should be the preferred access choice in elderly ACS patients undergoing PCI.
Third, new generation DES must be preferred over bare metal stents (BMS) in elderly ACS patients post-PCI. The SENIOR RCT including patients ≥75 years undergoing PCI showed that DES and a short duration of DAPT have better outcomes for all-cause mortality, MI, stroke, and ischemia-driven target lesion revascularization at 1 year as compared to BMS with similar duration of DAPT (RR 0.71; 95% CI [0.52–0.94]; p=0.02).71
Fourth, elderly patients should be recruited in cardiac rehabilitation (CR) or a secondary prevention program after ACS. CR, a comprehensive lifestyle program promoting physical activity, education, diet, weight control, risk reduction and adherence reduces cardiovascular morbidity and mortality, and improves exercise capacity and quality of life in elderly patients with cardiovascular disease. For frail elderly patients, emphasis should be given to their physical efficiency assessed by aerobic capacity (cardiopulmonary exercise test, and 6-minute walking test), on functional autonomy and on improvement of muscular strength, balance and flexibility (short physical performance battery).72 Tailored CR programs based on individual functional status are needed to manage the complexities of elderly patients with frailty. MACRO (NCT03922529) is an ongoing RCT that is addressing issues related to aging as a means to better facilitate CR.
Finally, pharmacological secondary prevention is an important part of management of elderly patients post ACS. Of note, there has been a decline in the rate of statin use in elderly patients post ACS with increasing age, particularly in those >75 years, reflecting differences in both prescribing and compliance.73 According to 2018 ACC/AHA guidelines, (level of evidence B–R) it is reasonable to initiate moderate or high-intensity statin and to continue high intensity statin (level of evidence C–LD) in elderly patients (>75 years) with clinical atherosclerotic cardiovascular disease (ASCVD) for secondary prevention (class IIa recommendation).74 The decline in statin use in the elderly may be due to the adverse effects of statin especially myopathy which is more common in elderly patients due to increased drug interactions and comorbidities. In such cases, using a lower dose, switching to an alternative statin or alternate-day dosing can be used which has shown equal efficacy in lowering LDL cholesterol with less risk of myopathy.75
Adequate control of blood pressure and diabetes is essential for secondary cardiovascular prevention. According to the 2017 ACC/AHA guideline on hypertension, (class IIa, level of evidence C – expert opinion) clinical judgement, patient preference, and a team-based approach to assess risks and benefits is reasonable for decisions regarding intensity of blood pressure-lowering therapy and choice of antihypertensive drugs for elderly patients ≥65 years with hypertension, a high burden of comorbidity, and limited life expectancy.76 Similarly, lenient HbA1c goals of 7–7.9% are recommended in elderly people ≥65 years, especially with frailty and multiple comorbidities.77
Current Guidelines and Future Guidance
The 2013 ACC/AHA and 2017 ESC guidelines do not include an age criterion for urgent reperfusion in STEMI.41,42 Thus, elderly patients with STEMI are treated with primary PCI where indicated regardless of age. The 2014 ACC/AHA guidelines recommend that older patients with NSTEMI should be treated with guideline-directed medical therapy, an early invasive approach and revascularization as appropriate.1 The 2020 ESC guidelines recommend the management of elderly patients with NSTEMI should be based on evaluation of ischemic and bleeding risks, life expectancy, presence of other comorbidities, the need for non-cardiac surgery, quality of life, presence or absence of frailty, cognitive status and functional impairment, values and preferences of patients, as well as the estimated risks and benefits of revascularization.60 Despite these guidelines, elderly patients are less likely to undergo invasive procedures compared to the younger population due to concerns of increased risk of complications, and larger RCTs evaluating early invasive therapies are needed in elderly patients with ACS while accounting for their comorbidities, functional status, and quality of life.
Conclusion
Older people constitute an increasing proportion of patients presenting with ACS. Their management is often challenging due to several factors including increased risk of complications. Urgent reperfusion with primary PCI is the standard of care in patients with STEMI irrespective of age. However, in elderly patients with NSTEMI, management depends on individual risk assessment. Recent studies have shown improved cardiovascular outcomes from an early invasive approach in these patients. However, these results are not generalizable to all elderly patients due to the very selective patient population included in these trials and confounding due to comorbidities and frailty. Future clinical trials including these parameters are needed to establish the definitive standard of care for management of elderly patients with NSTEMI.