Reperfusion of blood flow in the infarct-related artery through percutaneous coronary intervention (PCI) or fibrinolysis is the standard of care for the treatment of patients with ST-elevation MI (STEMI). When performed promptly, PCI is the preferred approach for reperfusion therapy in most patients with STEMI.
In a meta-analysis of 23 randomized trials comparing PCI with fibrinolytic therapy, there was a significantly lower risk of short-term death, stroke, or nonfatal MI in those who received PCI.1 In patients with suspected STEMI, several quality improvement measures have been undertaken to reduce the door-to-balloon (D2B) time, that is, the interval between patient arrival at the hospital to balloon angioplasty of the occluded coronary artery. Outcomes such as myocardial blush grade, ST-elevation resolution, mortality at 1 year, and heart failure at 1 year were all significantly lower in patients with expedited symptom onset-to-balloon inflation (OTB) time and D2B time.2
This article aims to examine the impact of the coronavirus disease 2019 (COVID-19) pandemic on OTB time and D2B time, identify factors that delay both OTB and D2B times and strategies that can help decrease these times. Before the pandemic, shorter D2B and OTB times were associated with mortality benefits. It is important to determine if shorter ischemic time means mortality benefit in the COVID-19 era and to identify possible strategies to shorten the ischemic time during the on-going pandemic. We will discuss evidence showing improved outcomes with shorter D2B times and the impact of COVID-19 on OTB and D2B times.
Methods
This review was conducted based on an established literature review protocol that detailed our objectives, methods, and selection criteria.3 The criteria for the selection of studies allowed the inclusion of many study designs, types of participants, interventions and outcome measures. We conducted electronic searches of the MEDLINE/PubMed and EMBASE databases to identify all relevant and pertinent articles. The included keywords were ‘Strategies Improving Door-to-Balloon Time’ or ‘Door to Balloon Alliance,’ ‘Improving Door to Balloon Time’ in conjunction with ‘STEMI,’ ‘PCI,’ ‘COVID-19,’ ‘SARS-CoV-2’ and ‘Review.’ References from chosen articles were also reviewed for possible selection per our selection criteria. The search was directed to identify articles discussing the significance of D2B times in the COVID-19 era, pre-COVID-19 era, and factors that impacted D2B times. Finally, all authors participated in the search and review of search results with a qualitative summary of relevant full-text versions of selected articles. Articles chosen for inclusion were consistent with our search parameters and published from the initialization of the database to December 1, 2020. Our literature review was limited to articles published in English, but not limited by country of origin.
Results
Evidence Supporting Benefits of Reducing Door-to-balloon Time
The significance of optimized management (angioplasty) of patients with STEMI and reduced D2B time has been well established. In 1999, Berger et al. showed that patients randomized to PCI in 60 minutes or less had the lowest rates of 30-day mortality, with rates progressively higher with an increased delay between diagnosis and balloon inflation.4 De Luca et al. expanded on this work, looking at 1,791 STEMI patients in a similar timeframe and concluded that for every minute of ischemic time until adequate reperfusion therapy, mortality at 1 year increased significantly.2
It is difficult to create objective guidelines about the timing of reperfusion therapy because there is great variability in total time from patient symptom onset to hospital arrival. Cannon et al. sought to address this issue and looked at the relationship between both OTB time and D2B time. Mortality in a cohort of 27,080 patients undergoing primary angioplasty was not related to OTB time, but there was a significant increase in mortality risk (by 41–62%) if D2B time exceeded 2 hours.5 Later studies that looked at the timeliness of reperfusion therapy found that when D2B time was <90 minutes, patients had significantly lower 30-day mortality and 1-year mortality.6,7 An analysis of 5,243 patients with documented STEMI from November 2011 to December 2015 indicated a lower risk of mortality associated with each 30-minute decrement in D2B time, with the greatest benefit seen in D2B times of <60 minutes.8 With the increased use of quality improvement initiatives such as the National Cardiovascular Data Registry (NCDR), there has been even greater scrutiny and analysis of outcomes after PCI. A study by Park et al. of 96,738 patients undergoing primary PCI for STEMI demonstrated a significant reduction in D2B time from 83 minutes to 67 minutes over 4 years, but did not demonstrate a significant reduction in in-hospital mortality (5.0% versus 4.7%, p=0.340).9
The discrepancies between these two analyses may be caused by multiple factors. Namely, the Park et al. study was a primarily Korean cohort, whereas the NCDR analysis was based on a US cohort. In the US cohort, the study population on average was older, had a higher BMI, and included a higher proportion of female patients.8,9 Furthermore, the reduction of D2B time in the NCDR analysis was only 16 minutes, whereas in the Park et al. study, outcomes were based on 30-minute increments. Lastly, it is important to note that time from symptom onset to when the patient presented to the hospital was collected for each patient, but no specific analysis was performed regarding OTB time in the NCDR registry. Hence, the NCDR data do not have the granularity of distinguishing OTB time compared with the Park et al. study.8,9
While there are conflicting data regarding the significance of OTB time compared with D2B time, it is important to minimize the ischemic time for a patient with STEMI.4,5 The D2B time appears to be a better quality-of-care indicator because the OTB time includes variation in patient presentations, and possible recall bias that is present when a patient is describing the timing of onset of their symptoms. It is difficult to make empirical recommendations based on the literature, but there are sufficient data to suggest that mortality increases as the time to balloon angioplasty increases.10
National Quality Improvement
With the overwhelming evidence that reductions in D2B times improve long-term outcomes for patients presenting with STEMI, it became imperative to formulate a unifying initiative. In 2006, the D2B Alliance was formed by over 1,000 hospitals across the US, with the goal of achieving D2B times of <90 minutes in at least 75% of non-transferred patients with STEMI.11 The D2B Alliance represents the first national quality improvement initiative from the American College of Cardiology’s (ACC) Quality Improvement for Institutions Program. The program was based on the results of the Acute Myocardial Infarction Guidelines Applied in Practice (AMI-GAP) initiative in Michigan, which was a systems-based approach to improving outcomes after AMI in a consortium of five hospitals in south-east Michigan.12 This project demonstrated that system-wide approaches to implement evidence-based medicine could improve outcomes. As a result, several of the strategies implemented in problem solving for the AMI-GAP project were used in the D2B initiative.
The D2B Alliance called for a multidisciplinary approach to quality improvement and needed buy-in from providers at all levels and in various settings. Specifically, five suggestions were outlined for hospitals to implement with the hope that addressing these bottlenecks could streamline activation of the cardiac catheterization laboratory (CCL) for patients with acute STEMI. These proposals included allowing for emergency department activation of the CCL without cardiologist approval, a single call activation of the CCL, CCL staff arriving on-site within 30 minutes of the call for activation, and rapid feedback that allowed for realtime performance measures and feedback to be given post-PCI. This, in conjunction with vocal support by senior management at the D2B Alliance hospitals, led to a significant reduction in D2B time, which is reflected in hospital reports of increased use of these measures. Other suggestions included allowing for CCL activation using ECGs from the field, but adoption of this metric was optional.13,14 The D2B Alliance met its goal in 2008 and, since then, additional studies have begun calling for D2B times of under 60 minutes.8
Current ACC/American Heart Association guidelines suggest that when a STEMI patient is directly being transferred to a PCI-capable center, then first medical contact to the deployment of the device in the procedure should be accomplished in 90 minutes; and if the patient is being transferred from a non-PCI capable center, then it should be accomplished in 120 minutes.15 European Society of Cardiology (ESC) guidelines suggest identical timings for D2B time.16 According to the ESC, time from STEMI diagnosis to passing of wire should be within 60 minutes if the patient presented to a PCI-capable facility, 90 minutes for a patient getting transferred to a PCI-capable facility, and should not be delayed >120 minutes if PCI is the primary strategy for treatment of STEMI.
Impact of COVID-19 on Door-to-balloon Time
During the on-going COVID-19 pandemic, STEMI management deserves special scrutiny. It is an established phenomenon that severe acute respiratory syndrome coronavirus 2 has an impact on the heart, whether directly or indirectly. Early studies from China made it clear that patients who had pre-existing cardiovascular disease, diabetes and hypertension died most often or were most often admitted to the intensive care unit as a result of COVID-19 infection.17 Here we will review the impact of COVID-19 on timings of presentation in patients with STEMI (Table 1) who underwent PCI.
An early paper from Yerasi et al. described the risks and benefits of PCI and fibrinolysis in STEMI patients during COVID-19 infection and proposed that PCI should still be the preferred modality in STEMI patients during the pandemic.18 As discussed earlier, there is sufficient evidence in the literature that reduction in D2B times improves long-term outcomes in STEMI patients. There has been concern about the impact of COVID-19 infection on D2B times in STEMI patients and the implication it will have on the prognosis of these patients.
In the literature, mixed results were found on the impact of COVID-19 infection on D2B times. A study from Ohio by Hammad et al. looked at 143 STEMI cases that presented from January to April 2020 in 18 hospitals.19 They found that, on average, D2B times were not different between the pre- and post-COVID-19 cohorts (59 minutes [44–84] versus 58 minutes [42–102]; p=0.84). However, they found that STEMI patients who presented 12 hours after the onset of symptoms had significantly high D2B time and peak troponins.
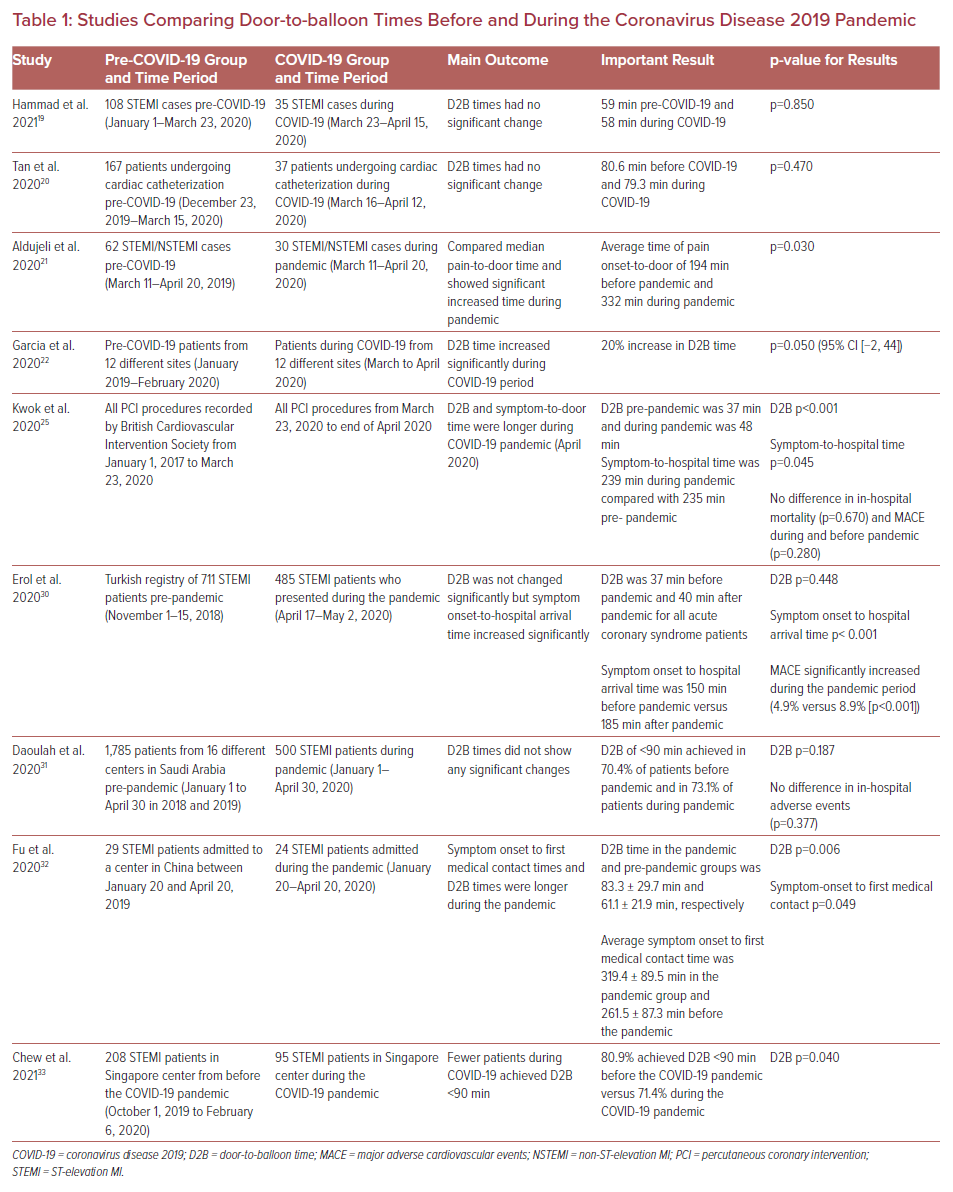
Similarly, a study from a single center in California by Tan et al. found that during the early months of the pandemic, patients did not seem to have delays in STEMI presentation or significant differences in all-cause mortality at their institution, compared with the pre-COVID-19 era.20 Another study from Texas by Aldujeli et al. that looked at 200 acute STEMI cases found that there were significant delays in onset to reaching the hospital in the STEMI patients after COVID-19 but, once in the hospital, D2B time was no different from the pre-COVID-19 era.21
In contrast, a study of data about STEMI patients from 18 hospital systems across the US performed by Garcia et al. found opposite results.22 They compared STEMI patients before COVID-19 (from January 2019 to February 2020) with STEMI patients during the COVID-19 pandemic (from March and April 2020) and found that the average monthly D2B time during the COVID-19 pandemic was about 20% (95% CI [−0.2, 44.0]; p=0.052) higher. Interestingly when they did monthly analysis, D2B times in March 2020 were increased by 27% (95% CI [6–52]; p=0.011), relative to pre-COVID-19 times, but no significant change was seen in D2B in April 2020.
Such mixed results of D2B times in the US are consistent with what has been seen in other countries. The OTB time delay has been reported across several European countries, including Italy, Spain, UK, Austria, Belgium, and Switzerland.23–27 Some studies have specifically also found delays in D2B times, while others have only found this with OTB times. For instance, Secco et al. carried out a study involving three high-volume centers in northern and central Italy and looked at all acute coronary syndrome cases in March 2019 compared with March 2020.28 In their STEMI subgroup they found that D2B (66 ± 17 minutes versus 40 ± 12 minutes, p<0.001) and OTB times (5.8 ± 3.1 hours versus 3.9 ± 2.2 hours, p<0.001) were significantly longer in March 2020 compared with 2019. They also found that patients who presented during the pandemic had high troponin values and lower residual left ventricular function on average, and higher predicated in-hospital and 6-month mortality values.28
A study from the UK by Kwok et al. found similar results.25 A large database of 34,127 patients with STEMI was studied. They compared patients who underwent primary PCI for STEMI in the years 2017 to 2019 with patients who had PCI for STEMI in the period from January 2020 to the end of April 2020. They found that, on average, after the lockdown period, D2B increased to 48 minutes from 37 minutes before the pandemic (48 minutes [21–112] versus 37 minutes [16–94]; p<0.001). Time from symptom onset to presentation at hospital also showed longer delays (150 minutes [99–270] versus 135 minutes [89–250]; p<0.001).25 However, there were no differences in in-hospital mortality and major cardiovascular adverse events. All studies demonstrated a significantly longer time from symptom onset to arrival at the hospital.
Likewise, in Asian and Middle-Eastern countries, such as China, Singapore, Turkey and Saudi Arabia, consistent delay in D2B and symptom onset to PCI time were observed.29–33 A study by Fu et al. showed that D2B time in the COVID-19 era was 83.3 minutes, which is significantly longer than 61.1 minutes from pre-COVID-19 (p<0.050).32 Similarly, symptom onset to hospital time was delayed in the COVID-19 era to 319.4 minutes from 261.4 minutes in the pre-pandemic period.32 A study from Singapore by Chew et al. looked at 323 STEMI cases that presented to tertiary care hospitals. They found that there were fewer patients who achieved D2B of <90 minutes during the COVID-19 outbreak, compared with patients from 2019 (71.4% versus 80.9%, p=0.042).33
Oddly enough, only patients with STEMI in South Korea (compared with other studies from all over the world) had better D2B during the COVID-19 outbreak. In the study by Lee et al., data about COVID-19 patients were analyzed over 20 weeks, starting January 26, 2020.34 All the patients with AMI who underwent PCI during the COVID-19 pandemic had longer D2B times (34.3 ± 11.3 minutes versus 22.7 ± 8.3 minutes; p<0.001) compared with patients pre-COVID-19. These data were from a single 560-bed hospital located in the Seoul metropolitan area. The authors of this study attributed these findings to smaller patient volume and increased availability of procedure rooms during the COVID-19 outbreak.
Discussion
Factors Affecting Door-to-balloon Time in the COVID-19 Era
To the best of our knowledge, there are no studies from the US that have specifically focused on elucidating factors that impacted D2B times in STEMI patients. However, we can infer different factors affecting OTB time and D2B in the COVID-19 era from various studies.
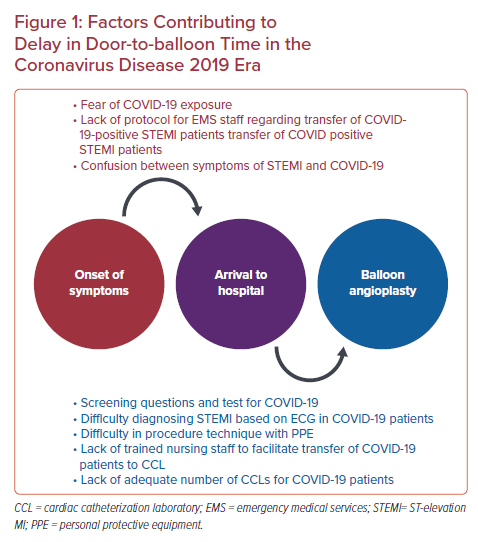
There are many possible reasons for delay from the onset of symptoms to reaching the hospital in STEMI patients (Figure 1). Patients may have been afraid of exposure to COVID-19 infection if they went to the hospital. Another possibility is that appropriate training of emergency medical services staff about how to appropriately triage or transfer patients with STEMI in the COVID-19 pandemic was lacking. Additionally, some patients may have confused symptoms of COVID-19 and STEMI. Delays could also have been a result of new requirements for screening questionnaires or performing tests, such as rapid COVID-19 test, transthoracic echocardiogram, or CT of the chest, to determine if a STEMI patient has COVID-19. Some possible reasons that led to delays specifically in D2B seen during pandemics are discussed here.
Some emergency department physicians faced difficulty in quickly diagnosing STEMI in patients with COVID-19 because of its presentation mimicking STEMI. If a hospital system was unprepared in advance to deal with a surge of COVID-19 cases and lacked a designated CCL for COVID-19 positive patients and trained staff that are specifically responsible for COVID-19 cases, it could delay D2B significantly. Another possibility is of hospitals only having one CCL for COVID-19 patients because, in such a case, a CCL would need proper sanitizing before the arrival of the next patient. Also, it is important to note that extra personal protective equipment on the operator can make performing angioplasty challenging.12,22,23,27,31
Strategies to Reduce Door-to-balloon Time in the COVID-19 Era
Education is key to reducing D2B, especially in the COVID-19 era. Emergency medical services staff require proper training and the public must be aware of the need to seek prompt medical attention for signs or symptoms of a heart attack. Education campaigns in the local community, with the help of social media and education of patients by primary care physicians, can help in reducing the fear of contracting COVID-19 infection.
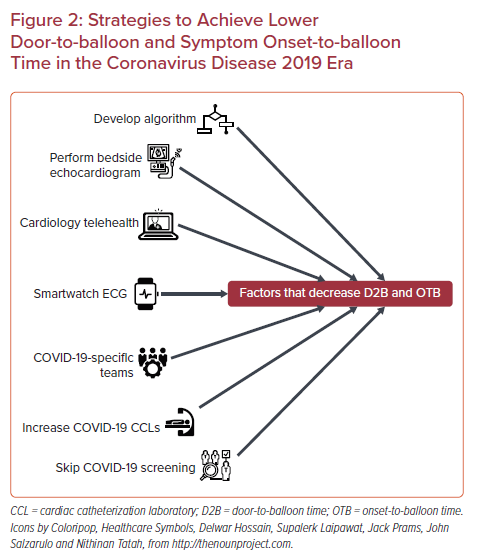
Some potential solutions (Figure 2) to reduce D2B time specifically in the COVID-19 era are:
- Develop an algorithm for the regional hospital network of how to transfer STEMI patients suspected of having COVID-19 to the CCL.
- Assign teams that are specifically responsible for COVID-19 cases.
- Assign two or more CCLs for COVID-19 cases.
- Perform bedside echocardiography to quickly assess the patient and reduce the exposure of the technician.
- Consider bypassing COVID-19 tests in urgent cases.
- Train nursing staff on how to safely transfer COVID-19 patients with STEMI to the CCL once they are in the hospital.
- Where a standard 12-lead ECG might not always be available, a wearable smartwatch device with the capability to recognize STEMI with multiple-lead ECGs would be a great alternative.35
- Develop an on-call telehealth cardiology team that specifically helps with timely diagnosis and CCL activation.17, 22,27,30,31
Limitations
One of the limitations of this review is the method used in the selection of the articles. To provide a concise review, some important articles were inevitably unable to be included. As the main topic involves a discussion about the impact of COVID-19 infection, most of the studies reviewed have a small population size and results cannot be extrapolated to long-term outcomes or any other topic.
Conclusion
For patients presenting with STEMI, PCI is the gold standard treatment modality. Studies have shown that reducing D2B and OTB times have significant mortality benefits. The COVID-19 pandemic has adversely affected OTB times, yet mixed results have been found concerning the D2B times and mortality in patients. Further studies with larger sample size and longer follow-up are needed. Given the known mortality benefit with low D2B times, it is imperative to continue to develop strategies to reduce ischemic time in the current era.