Historically, HDL cholesterol (HDL-C) has been inversely associated with adfverse cardiovascular outcomes such as MI, stroke, and cardiovascular death.1–3 This led to widespread belief that HDL-C, in addition to LDL cholesterol (LDL-C), was a modifiable risk factor for cardiovascular disease.
However, efforts to increase HDL-C in high-risk patients with well-controlled LDL-C values have not demonstrated a reduction in adverse cardiovascular outcomes.4,5 These have included the administration of cholesteryl ester transfer protein (CETP) inhibitors, which dramatically raise HDL-C, but have failed to demonstrate a meaningful reduction in adverse cardiovascular events.6–9
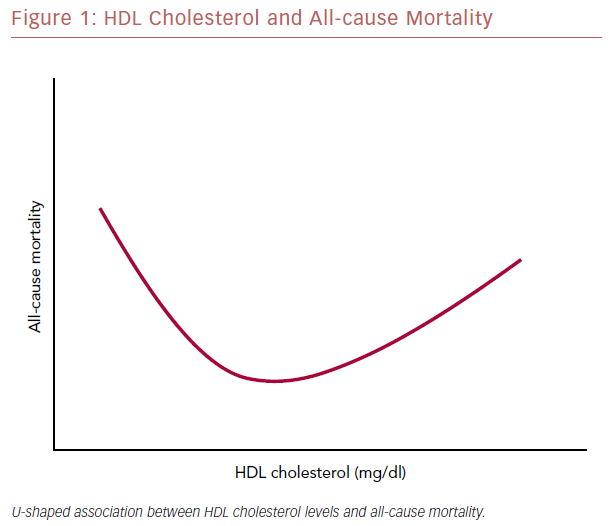
Subsequent analyses of several large population cohorts suggested a plateauing of the inverse association between HDL-C and adverse cardiovascular events at high levels of HDL-C. More recently, a U-shaped association has been demonstrated between HDL-C and adverse events, including all-cause mortality, suggesting that, at very high levels, HDL-C may correlate with increased cardiovascular events and all-cause death.
The aim of this article is to outline the data regarding very high HDL-C and adverse outcomes, to explore potential explanations for this seemingly paradoxical association, and to provide clinically relevant applications.
Exploring HDL Cholesterol and Adverse Outcomes
Assessment of HDL Cholesterol and Cardiovascular Risk in Large Population Cohorts
Identification of HDL-C as a potential protective factor in atherosclerotic cardiovascular disease (ASCVD) gained significant attention after analysis of the Framingham Heart Study cohort. This study demonstrated an inverse association between HDL-C levels and incidence of CHD in more than 2,800 men and women without known cardiovascular disease after a follow-up of 12 years.1 These findings remained significant after multivariate adjustment for other common cardiovascular risk factors including tobacco use, hypertension, obesity, and age.1 Of note, however, HDL-C categories for analysis were broken into quartiles (<1.04 mmol/l, 1.04–1.27 mmol/l, 1.30–1.53 mmol/l, and >1.55 mmol/l), which may have limited the ability to detect adverse outcomes in a small subset of patients with very high HDL-C values.
Analysis from the more recent Emerging Risk Factor Collaboration, a combination of 68 long-term prospective cohorts involving over 300,000 individual patient records from across the world, supported this inverse linear association between HDL-C and adverse cardiovascular events.3
When the population was separated into quintiles, there was notable attenuation of the inverse relationship between HDL-C and adverse cardiovascular events among patients in the highest quintile.3 However, it is challenging to draw definite conclusions from this study as it involved analysis from numerous prospective studies with differing inclusion and exclusion criteria as well as recorded covariates.
Analysis of the Multi-Ethnic Study of Atherosclerosis (MESA) cohort provided one of the first signals that very high HDL-C may be correlated with adverse cardiovascular outcomes.10 The study included more than 5,500 community-dwelling men and women at low inherent risk for cardiovascular disease and excluded those on cholesterol-lowering medication. Initial analysis of HDL-C levels (broken down into quartiles) and CHD event rate suggested an inverse linear relationship as had been demonstrated previously.10 However, a fifth HDL-C category of >2.07 mmol/l was analyzed separately and was notable for an increased risk of CHD events (HR 2.59; 95% CI [1.11–6.02]) compared to the reference HDL-C range.10 While these results remained significant after multivariate regression, alcohol intake was not included in the adjustment, which is a potential confounder as alcohol is associated with both increased HDL-C and adverse events.
Very High HDL Cholesterol and Adverse Events in Patients at Low Risk of Cardiovascular Disease
Given that HDL-C values >2.07 mmol/l are relatively rare among people at low risk of cardiovascular disease, it was hypothesized that much larger patient samples would be necessary to confirm a significant association between very high HDL-C and adverse cardiovascular events.
The Cardiovascular Health in Ambulatory Care Research Team (CANHEART) dataset, which involves more than 600,000 individuals from Ontario, Canada, without known cardiovascular disease, was analyzed after a median follow-up of 5 years in an attempt to understand the relationship between HDL-C and cause-specific mortality.11
The results demonstrated a statistically significant increased risk of all-cause mortality in men with HDL-C levels >2.07 mmol/l and HDL-C levels <0.78 mmol/l compared to reference HDL-C levels of 1.04–1.30 mmol/l, after adjusting for covariates including heavy alcohol use.11 Interestingly, this significant increase in mortality for HDL-C values >2.07 mmol/l was driven by non-cardiac, non-cancer related deaths, although there was a non-significant trend towards an increased risk of cardiac death.11 There was no statistically significant increase in all-cause mortality in women in the highest HDL-C category (>2.33 mmol/l) but there was a significant increase in non-cancer, non-cardiac associated death.11
While this analysis of the CANHART dataset did not include major adverse cardiovascular events as an endpoint, the higher non-cardiac death rates observed in patients with very high HDL-C levels is surprising. This could reflect a limitation of analyzing mortality rates in a large dataset, as cause-specific mortality was obtained from patient death certificates, which can misclassify the cause of death. Alternatively, these findings could support that the HDL molecule is crucial to broader systemic pathophysiologic processes.
Perhaps the best evidence to date detailing the link between very high levels of HDL-C and increased adverse events comes from an analysis of two general population cohorts in Copenhagen, Denmark.12 The Copenhagen City Heart Study and the Copenhagen General Population Study cover two longitudinal, non-overlapping cohorts at a relatively low risk for cardiovascular disease. The two cohorts were analyzed in combination to generate a population sample of more than 50,000 men and 60,000 women who were followed for a median of 6 years. Primary endpoints included all-cause mortality and cardiovascular death. Secondary endpoints included incidence of ischemic heart disease, MI, and ischemic stroke. When HDL-C was assessed as a continuous variable using restricted spline curves, there was a significant ‘U-shaped’ association with all-cause mortality in both men and women (Figure 1), although the association was stronger in men.
Analysis of HDL-C categories demonstrated a significantly increased risk of all-cause death at HDL-C values of >2.51 mmol/l in men (HR 1.36; 95% CI [1.09–1.70] and >3.50 mmol/l in women (HR 1.68; 95% CI [1.09–2.58] 95%) as well as <1.04 mmol/l in both sexes compared to the lowest risk HDL-C categories for each sex. Cardiovascular death was also demonstrated to have a U-shaped association with HDL-C values in both men and women. The risks of CHD, MI, and ischemic stroke were not significantly greater in the highest HDL-C categories than in reference values, although there was a plateauing of the inverse relationship between these variables at very high HDL-C levels.12
All findings remained significant after multivariate adjustment, which included degree of alcohol use, hormone replacement therapy for women, and physical activity level, all of which have previously been shown to increase HDL-C levels.13–15 Further sensitivity analysis stratifying alcohol use did not demonstrate a significant difference in the results previously stated. These data provide compelling evidence of an epidemiologic link between very high HDL-C levels and both all-cause death and cardiovascular death in a low-risk population.11,16
While the study involved a rather homogenous population in one geographic area, this U-shaped association was also noted in the CANHEART study in Ontario, Canada, described above, and in a more recent population-based study from Japan, suggesting generalizability to low-risk populations across the globe.11,16
Very High HDL Cholesterol and Adverse Events in Patients at High Risk of Cardiovascular Disease
The majority of data linking very high HDL-C levels and adverse events have been obtained in populations at relatively low risk for cardiovascular disease, and data in higher risk individuals are limited.
Van der Steeg et al. analyzed the association between HDL-C and adverse cardiovascular events in two distinct populations – the Incremental Decrease in End Points Through Aggressive Lipid Lowering trial (IDEAL) and EPIC (European Prospective Investigation of Cancer)-Norfolk cohorts.17 The IDEAL cohort involved 8,888 patients with a prior coronary event randomized to receive high-intensity versus moderate-intensity statin therapy. EPIC-Norfolk was a cohort at low risk for cardiovascular disease and involved patients enrolled at community practices in Norfolk, UK.
Analysis of these two cohorts included all 8,888 patients from IDEAL and a 1:2 case-control study of the EPIC-Norfolk cohort involving those who developed coronary artery disease (CAD) during the follow-up period (858 patients) and matched controls (1,491 patients). Results were broken down by cohort. In the IDEAL cohort, there was an increased risk of the combined primary endpoint of coronary death, non-fatal MI, and resuscitation after cardiac arrest in patients with HDL-C levels <1.04 mmol/l and >2.07 mmol/l compared to the lowest risk HDL-C range (1.55–1.80 mmol/l) after adjusting for common risk factors (this did not include alcohol use).17
In the EPIC-Norfolk cohort, there was an inverse association between HDL-C values and the primary endpoint of fatal or non-fatal CAD after adjusting for common risk factors (excluding alcohol use). These data may suggest that patients with prior cardiovascular disease and very high HDL-C levels are at higher risk for subsequent events than patients with similar HDL-C levels who are at lower cardiovascular risk at baseline. However, limitations in this two-cohort analysis include differing study design involving two different primary endpoints, and the lack of adjustment for alcohol use in the IDEAL cohort. Furthermore, there was no analysis of mortality data, which has demonstrated the strongest correlation with very high HDL-C levels as detailed above.
Recently, preliminary data presented at the European Society of Cardiology included 5,965 individuals enrolled in the Emory University cardiovascular biobank in Atlanta, Georgia, who had either known CAD or were at high risk for cardiovascular disease, who were followed for a median of 3.9 years to assess the relationship between elevated HDL-C levels and adverse events.18 The two co-primary endpoints were a combination of cardiovascular death or non-fatal MI and all-cause mortality. Results demonstrated there was a U-shaped association between HDL-C levels and both all-cause mortality and cardiovascular death or non-fatal MI when using restricted cubic spline regression.18 There was a significantly increased risk of all-cause mortality at HDL-C levels of >2.07 mmol/l and <1.17 mmol/l, and an increased risk of the combination of cardiovascular death and non-fatal MI at HDL-C levels >2.60 mmol/l and <1.17 mmol/l after adjustment for common covariates including alcohol use.18
These data, albeit preliminary, suggest there is a correlation between very high HDL-C levels and all-cause mortality in a high-risk population, adding to a growing evidence base. Given the U-shaped association between these two variables, two important questions arise:
- Is this correlation causative?
- What are potential explanations for this finding?
Possible Explanations for the HDL Paradox
Genetic Variants Associated with Elevated HDL-C
Several gene mutations associated with altering HDL-C levels in vivo have been identified.19 CETP facilitates the exchange of cholesteryl esters for triglycerides between HDL and remnant lipoproteins. Inhibition of this action leads to significant increases in HDL-C, which has prompted several trials of pharmacological CETP inhibitors with the intention of reducing residual cardiovascular risk in patients at high risk. Unfortunately, these trials have not demonstrated a consistent reduction in cardiovascular risk, with one trial even suggesting an increased risk.6–9
Given the inconsistent results of these pharmacological trials, loss of function genetic mutations in the CETP gene that may translate to a similar increase in HDL-C have also been analyzed with mixed results. One study involving more than 9,000 community-dwelling men and women and over 900 men and women with ischemic heart disease found a significantly increased risk of ischemic heart disease in women only, with a specific single nucleotide polymorphism (SNP) of the CETP gene that led to a mild mean increase (~0.13 mmol/l) in HDL-C levels among the affected population.20 However, other SNPs of the CETP gene that lead to a similar mean increase in HDL-C have been found to have an inverse association with ischemic cardiovascular disease.21 It is important to note that these mutations of the CETP gene do not exclusively affect HDL-C values, and also lead to mild reductions in LDL-C, triglycerides, and apolipoprotein B. Therefore, the associations demonstrated may be confounded by these additional effects of CETP mutation.
To address this, deLemos et al. performed a genome-wide association study that identified several variants of the endothelial lipase gene (LIPG) that were exclusively associated with HDL-C.22 Of these variants, one particular loss of function SNP (Asn396Ser) was associated with significantly increased HDL-C and decreased endothelial lipase activity in vitro.23 As part of a Mendelian randomization analysis, carriers of this SNP of LIPG were found to have higher levels of HDL-C (mean 1.41 mmol/l) but similar levels of other lipids compared with non-carriers.24 In addition, carriers of the Asn396Ser SNP did not demonstrate any association with the risk of MI in a prospective cohort involving six population-based trials and more than 50,000 participants.24
Scavenger receptor class B type 1 (SR-BI) is a major receptor for HDL that promotes the transfer of cholesterol from the HDL molecule to the liver. Mutations of the SR-BI gene (SCARB1) have been found to be associated with increased HDL-C without significant association with other lipid measures.25 Among a population of >300,000 individuals, a specific SNP of SCARB1 (P376L) was found to be associated with significantly increased HDL-C levels, with a large effect size (beta = 0.22 mmol/l).25 A case-control analysis of 137,995 patients with and without CHD demonstrated a significantly increased risk of CHD in carriers of the P376L allele compared to non-carrier controls.25 However, this specific mutation was rare in the large population studied, limiting its general applicability to patients with very high HDL-C. A subsequent case-control analysis of 36,886 patients with identified CAD from the National University Hospital of Iceland and 306,268 control individuals from the Icelandic genealogical database did not demonstrate any association with CAD among carriers of three novel SNPs of the SCARB1 gene.26 Of note, the P376L mutation was not one of the three variants included in this analysis.26
The evidence to support a genetic cause of very high HDL-C and an association with adverse cardiovascular events is mixed. This outcome variability, at least in part, is likely to come from the different genes and numerous SNPs within the genes examined. Additionally, genes that also affect other risk factors for cardiovascular disease, such as CETP, provide limited evidence because of potential confounding. Furthermore, few studies used all-cause mortality as an endpoint. As the association between very high HDL-C and all-cause mortality has the strongest epidemiologic link, further investigation is needed.
HDL Function at High HDL-C Levels
Pursuit of the potential causative relationship between HDL-C and adverse events has shifted investigative attention to the function of the HDL molecule. At present, there are two main validated measurable assays of HDL function: the cholesterol efflux capacity (CEC); and the HDL inflammatory index.
CEC is a dynamic assessment of the rate and magnitude of cholesterol movement from the peripheral tissues to the liver, otherwise known as reverse cholesterol transport. This process is mediated by the HDL molecule, so impairment of CEC is suggestive of dysfunctional HDL. To date, several studies have demonstrated an inverse relationship between CEC and adverse cardiovascular events.27,28 Furthermore, CEC has been shown to be a superior marker for incident adverse cardiovascular events than HDL-C, and improves net reclassification indices for predicting cardiovascular risk in a primary prevention population.27,28 When analyzed in a population of patients with very high HDL-C levels (mean 2.23 mmol/l) and CHD, CEC was markedly impaired compared to age, sex, and HDL-C-matched controls.29 While these data suggest an inverse correlation between CEC and adverse cardiovascular events, likely outperforming HDL-C as an independent risk factor, they also elucidate whether CEC becomes impaired at very high levels of HDL-C exclusive of incident cardiovascular disease. A study by Agarwala et al. investigated a population of patients with very high HDL-C and CHD. HDL-C values were similar in matched controls free from cardiovascular disease and had superior CEC.29 Whether very high HDL-C levels affect CEC directly is unknown.
A second functional assessment of HDL, the HDL inflammatory index, measures the degree of LDL oxidation via a cell free assay (CFA) and LDL mediated monocyte chemotactic activity (MCA) as influenced by HDL compared to control LDL. Pro-inflammatory and pro-oxidant HDL will increase MCA and CFA values (>1.0) compared to control LDL (reference 1.0). Alternatively, anti-inflammatory and antioxidant HDL will decrease MCA and CFA values (<1.0). Ansell et al. conducted a small prospective study involving patients who presented with incident CHD and age- and sex-matched controls.30 The initial study group involved 26 patients with incident CHD and HDL-C values in the normal range compared to age and sex-matched controls. There was a marked increase in CFA and MCA values in the CHD experimental group compared to the controls (MCA 1.38 versus 0.38 p<1.5x10−5, CFA 1.19 versus 0.53 p<7.4x10–14).30
A second study group involving 20 patients with incident CHD and very high HDL-C values (>2.18 mmol/l) demonstrated a similar increase in CFA and MCA values in the experimental group (MCA 1.28 versus 0.35 p<1.7x10−14, CFA 1.37 versus 0.66 p<4.4x10−12).30 These data suggest that, in patients with established cardiovascular disease, HDL is more likely to be pro-inflammatory than in similar control populations. While this finding was demonstrated in a population of patients with very high HDL-C, the results are confounded by the presence of CHD. Statistical comparison of the two populations with incident CHD but different mean HDL-C levels was not completed, although raw data did not suggest a difference between these two groups.
HDL may play a role in immune system modulation, which could in part be tied to its pro- and anti-inflammatory properties.31 In patients with severe sepsis, HDL-C was inversely associated with other markers of systemic inflammation, and low levels of HDL-C were predictive of poor outcomes in a small prospective study.32 Recently, Madsen et al. analyzed the Copenhagen General Population Study and Copenhagen City Heart Study to understand the association between HDL-C and infection risk.33 The association between HDL-C and risk of any infectious disease was U-shaped, although the absolute highest risk for infectious disease remained at very low levels of HDL-C.A similar association was noted between HDL-C and death related to infectious disease.33 Other lipids measures, including LDL-C and triglycerides, did not share this U-shaped association.33 While these data provide evidence that HDL-C at extreme levels correlates with infectious disease risk, they do not provide a causative link.
Several other functions of the HDL molecule have been suggested by researchers, including roles in endothelial function, cellular apoptosis, and regulation of endothelial progenitor cells.34–36 While HDL clearly plays a role in many systemic processes in the human body, there is not significant data nor enough readily available measures of these functions to conclude that dysfunctional HDL causes adverse outcomes. Furthermore, no study to date has accurately assessed the functional status of the HDL molecule when HDL-C is at very high levels, despite recent data suggesting an association with increased infection risk at very high HDL-C levels. Therefore, the question of whether dysfunctional HDL is an explanation for the epidemiological association between very high HDL-C and adverse outcomes requires further exploration.
Residual Confounding
The association between very high HDL-C and other risk factors for adverse events has been studied insufficiently, leading to the possibility of residual confounding in the epidemiological studies described. While excessive alcohol use is one known risk factor that may confound results, this was adequately accounted for in several of the more recent population based studies, and is unlikely to be a sufficient explanation for the correlation between very high HDL-C and adverse events. However, there may be other risk factors, similar to alcohol, that are associated with both elevated HDL-C levels and adverse events but have not been identified and accounted for.
Conclusion
The inverse association between HDL-C and adverse outcomes has recently been challenged by the results of several large, population-based studies that have suggested that this relationship is instead U-shaped. These contemporary findings used large sample sizes to correctly power the studies to detect significant event rates in the small portion of the general population with very high HDL-C values. The findings suggest that very high HDL-C is correlated most with an increased risk of all-cause death, rather than cardiovascular death or adverse cardiovascular events. The understanding behind this epidemiologic link remains unclear. Possible explanations include genetic mutations linked to very high HDL-C, impaired HDL function at high levels of HDL-C, and the possibility of residual confounding. While several genes, when mutated, are associated with increased HDL-C – such as CETP, SCARB1, and LIPG – studies of patients who carry these mutated alleles have not demonstrated a clear increased risk of all-cause mortality or adverse cardiovascular events.
Whether the HDL molecule becomes dysfunctional at very high HDL-C levels still remains unknown. To date, no study has clearly linked very high HDL-C levels with impaired HDL function, despite available ways to assess HDL function, such as CEC and the HDL inflammatory index assays. The role of HDL in immune system modulation and infection regulation provides our best insight into a potential explanation. The results of a large retrospective analysis in Copenhagen, Denmark, suggest that very high (and very low) HDL-C levels correlate with both increased risk of infection and death related to infectious disease. This may provide insight as to why very high HDL-C levels correlate better with all-cause mortality than cardiovascular endpoints, but a causative link has not yet been proven.
Finally the possibility of residual confounding remains, given the lack of other definitive answers to this paradox. Given the complexity of the HDL molecule and the diverse roles it plays in the human body, using HDL-C as a tool for cardiovascular risk prediction may no longer be an effective clinical strategy, especially when HDL-C is significantly elevated. Use of other HDL-related measures, such as HDL particle concentration or apolipoprotein A1, or assessments of HDL function, such as CEC, may better predict adverse events.17,27,37
At present, given the limited data verifying a causative link between HDL-C and adverse events, pharmacological treatment of HDL-C, whether it is too low or perhaps too high, should not be considered an initial therapy for risk reduction. Until more is uncovered through research, patients should focus on modifying other well-established risk factors for cardiovascular disease, such as elevated LDL-C, hypertension, and smoking.