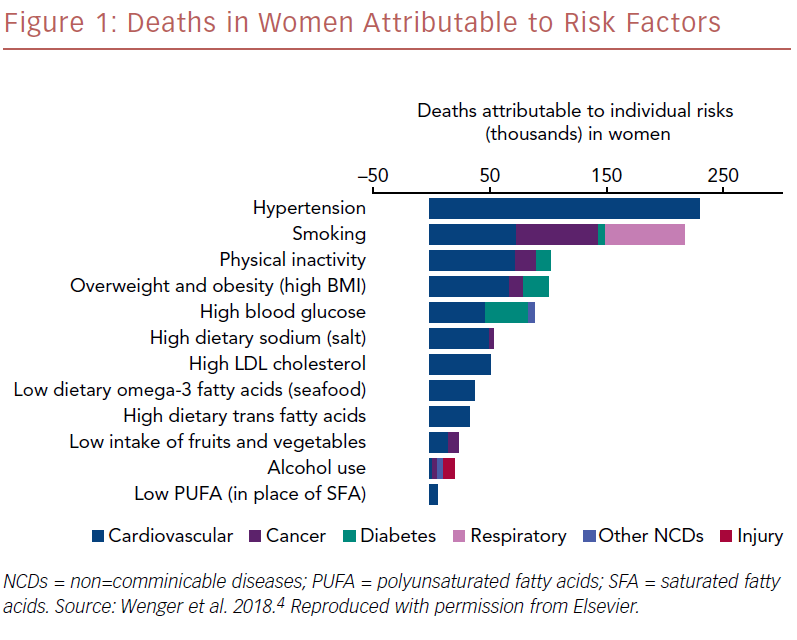
Hypertension was the leading cause of death worldwide in 2010 (Figure 1). Its scope is broad: hypertension and its sequelae account for the leading cause of disability-adjusted life years and for more cardiovascular deaths than any other modifiable cardiovascular risk factor, and 25% of all cardiovascular events can be attributed to hypertension.1–3
Targeting hypertension with early management is crucial for population and individual health and can improve cardiovascular outcomes. The prevalence of hypertension in the US alone is staggering. According to Wenger et al., 29% of all adults have hypertension, and it is present in 64.9% of people >60 years and 7.3% of those aged 19–39.4 These realities demonstrate a large population in which general practitioners can make real and effective change.
These trends are not confined to the US and there is also a high prevalence of hypertension in Europe. As in the US, there are regional variations in hypertension rates and its attendant cardiovascular morbidity and mortality, with eastern European countries still seeing higher disease prevalence and rates of modifiable risk factors. Targeted treatment of blood pressure in several European nations has led to a decline in mean systolic blood pressure (SBP) over the past four decades.5
The Importance of Treating Hypertension
The risk of cardiovascular disease increases significantly for adults with hypertension, and improving or eliminating this risk factor affects overall cardiovascular disease prevalence.
Research using data from the Cardiovascular Health Study and the Health, Ageing and Body Composition (ABC) study investigated 4,409 older people (mean age 72.9 years) who were based in the community, did not have heart failure and had not been treated with anti-hypertensives.6 Investigators looked at the primary outcome of first hospitalization for heart failure. Participants were divided into prehypertension (SBP 120–139 mmHg), stage 1 hypertension (SBP 140–159 mmHg), and stage 2 hypertension (SBP ≥160 mmHg). There was a continuous positive association between SBP and heart failure risk. More than half (51.7%) the incidents of heart failure were in people whose SBP was <140 mmHg. In a study of more than 10,000 adults followed from the age of 30 years, hypertension (SBP >140 mmHg) resulted in a higher lifetime risk of cardiovascular disease overall and heart failure in particular.7
Pharmacological treatment of hypertension has been clearly shown to result in real and sustained reductions in SBP and diastolic blood pressure (DBP) and improved primary and secondary outcomes.8,9 A meta-analysis of eight trials of blood pressure lowering as a determinant of cardiovascular outcome, which included 12,903 young patients (30–49 years old), 14,324 elderly (60–79 years old), and 1,209 very elderly (>80 years old), looked at the pooled results of using antihypertensive drugs against placebo or no treatment.10 Antihypertensive treatment reduced SBP/DBP by 8.3/4.6 mmHg in young patients, by 10.7/4.2 mmHg in older patients, and by 9.4/3.2 mmHg in very elderly patients, resulting in DBP:SBP lowering rations of 0.55, 0.39, and 0.32, respectively (p=0.004). Despite the differential lowering of SBP and DBP, antihypertensive treatment reduced the risk of all cardiovascular events, stroke and MI in the three age groups to a similar extent. Absolute benefit increased with age and with lowering of DBP:SBP ratio.
Similarly, the Systolic Blood Pressure Intervention Trial (SPRINT) involved 9,361 participants with an SBP > 130 mmHg and an increased cardiovascular risk without diabetes.11 They were divided into two groups: those who had a target SBP <120 mmHg were in the intensive treatment group, and those who had a goal of <140 mmHg were in the standard treatment group. Intensive treatment was found to be superior for the secondary outcomes of heart failure incidence (p=0.002), and death from cardiovascular disease (p=0.005). The primary composite outcome was MI, other acute coronary syndromes, stroke, heart failure, or death from cardiovascular causes, and intensive treatment also significantly reduced the incidence of these outcomes (p<0.001).
Non-Pharmacological Approaches to Reducing Blood Pressure
There are some non-pharmacological approaches to reducing blood pressure, including weight loss for patients who are overweight or obese, a heart-healthy diet, such as the Dietary Approaches to Stop Hypertension (DASH) diet, sodium reduction, potassium supplementation, increased physical activity, and a reduction in alcohol consumption.
Obesity is closely tied to hypertension; weight loss of 5–10% will lower blood pressure. Diet and physical activity are strongly related. A DASH diet can result in a BP that is 10 mmHg lower, while physical inactivity doubles a patient’s CVD risk. Similarly, increasing exercise can lower blood pressure by 5–8 mmHg and halve CVD risk.12
Primary and Secondary Prevention
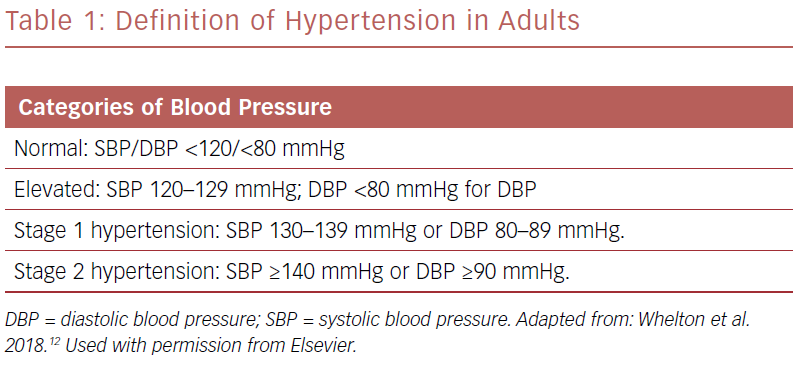
Primary prevention includes treating high-risk adults who have an estimated 10-year risk >10% of developing CVD and an SBP >130 mmHg or DBP >80 mmHg. Secondary prevention is treatment to avoid recurrent CVD events in patients that have clinical CVD and an SBP >130 mmHg or DBP >80 mmHg (Table 1).
Estimation of risk can be calculated using the Atherosclerotic Cardiovascular Disease (ASCVD) Risk Calculator.13 This uses pooled data to assess risk factors and guide treatment options. It is important to note that patients have multiple interrelated risk factors, some of which are modifiable, such as cholesterol levels, blood pressure, smoking, diabetes, obesity/sedentary lifestyle, and some of which are not, such as age, gender and family history. However, using a risk calculator with pooled cohorts can help to identify and stratify patients based on modifiable and non-modifiable risk factors.
Setting a Target
In patients with known CVD or a 10-year risk that is > 10%, the blood pressure goal would be <130/80 mmHg. In those patients who have an intermediate risk or do not have additional markers of increased CVD risk, a target of <130/80 mmHg is also reasonable.
Pharmacological Approaches
First-line agents for pharmacological treatment for hypertension include thiazide diuretics, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, or angiotensin receptor blockers (ARBs). Notably, none of these drugs have been shown to be clearly superior to another. In patients who fail to meet their blood pressure control target, combination drug therapy may be beneficial. Physicians can elect to use two first-line agents if the patient has stage 2 hypertension and has an average blood pressure of >20/10 mmHg above target. It is reasonable to use monotherapy if the patient has stage 1 hypertension with a blood pressure goal of <130/80 mmHg. Doses can be titrated accordingly with sequential addition of other agents to achieve target blood pressure.
Heart Failure
Hypertension poses a significant risk of heart failure. In fact, 75% of those with congestive heart failure have had antecedent hypertension.14 In those adults with an increased risk of heart failure, the optimal blood pressure for those with hypertension is less than 130/80 mmHg. In fact, large scale randomized controlled trials have shown that antihypertensive drug therapy reduces the incidence of heart failure in patients with hypertension. In the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) trial, chlorthalidone reduced the risk of heart failure with reduced ejection fraction (HFrEF) more than amlodipine and doxazosin, however it was similar to lisinopril.12,13 Of note, non-dihydropyridine calcium channel blockers, such as verapamil and diltiazem, have negative inotropy and are therefore not recommended for patients at risk of heart failure.
In the instance of heart failure with preserved ejection fraction (HFpEF), hypertension is prevalent in 60–90% of cases. Therefore, preventing hypertension and/or treating it is critical to reducing the prevalence of HFpEF. Treating hypertension in the setting of heart failure reduces hospitalizations, events, and mortality.15 Diuretics are among the most important agents for reducing blood pressure and improving the success of other agents. In the ALLHAT trial, chlorthalidone demonstrated a decreased incidence of new-onset HFpEF compared with amlodipine, doxazosin, and lisinopril.15
Patients with HFpEF who present with volume overload will require diuretics, which help to lower blood pressure. In persistent hypertension, despite improving volume status for those patients with HFpEF, ACE inhibitors, ARBs, or beta blockers can help reduce blood pressure to a target <130/80 mmHg.
Personalizing Hypertension Treatment Plans
In those patients who are 65 years or over, ambulatory and living in the community, the goal remains a SBP <130 mmHg. If older patients have a high burden of comorbid conditions, shared decision making with clinical judgement and a team-based approach are important. In black adults who do not have chronic kidney disease or heart failure, initial antihypertensive treatment includes a thiazide-type diuretic or a calcium channel blocker. Similarly, a drug regimen that includes two or more antihypertensives is recommended to achieve a blood pressure goal <130/80 mmHg, especially in black adults.12
Conclusion
Overall, early management and treatment of hypertension by general practitioners will improve cardiovascular outcomes. By adhering to the target blood pressure guidelines, assessing CVD risk, encouraging lifestyle changes, and recommending multiple drug regimens as indicated, general practitioners should feel empowered to make a real change in this patient group. In addition, by personalizing the approach depending on ethnicity and heart failure class, they can expect a reduction in cardiac events, hospitalizations, and overall negative outcomes.